Entamoeba histolytica is the causative organism of amoebiasis. It exists in two forms: cysts and trophozoites.
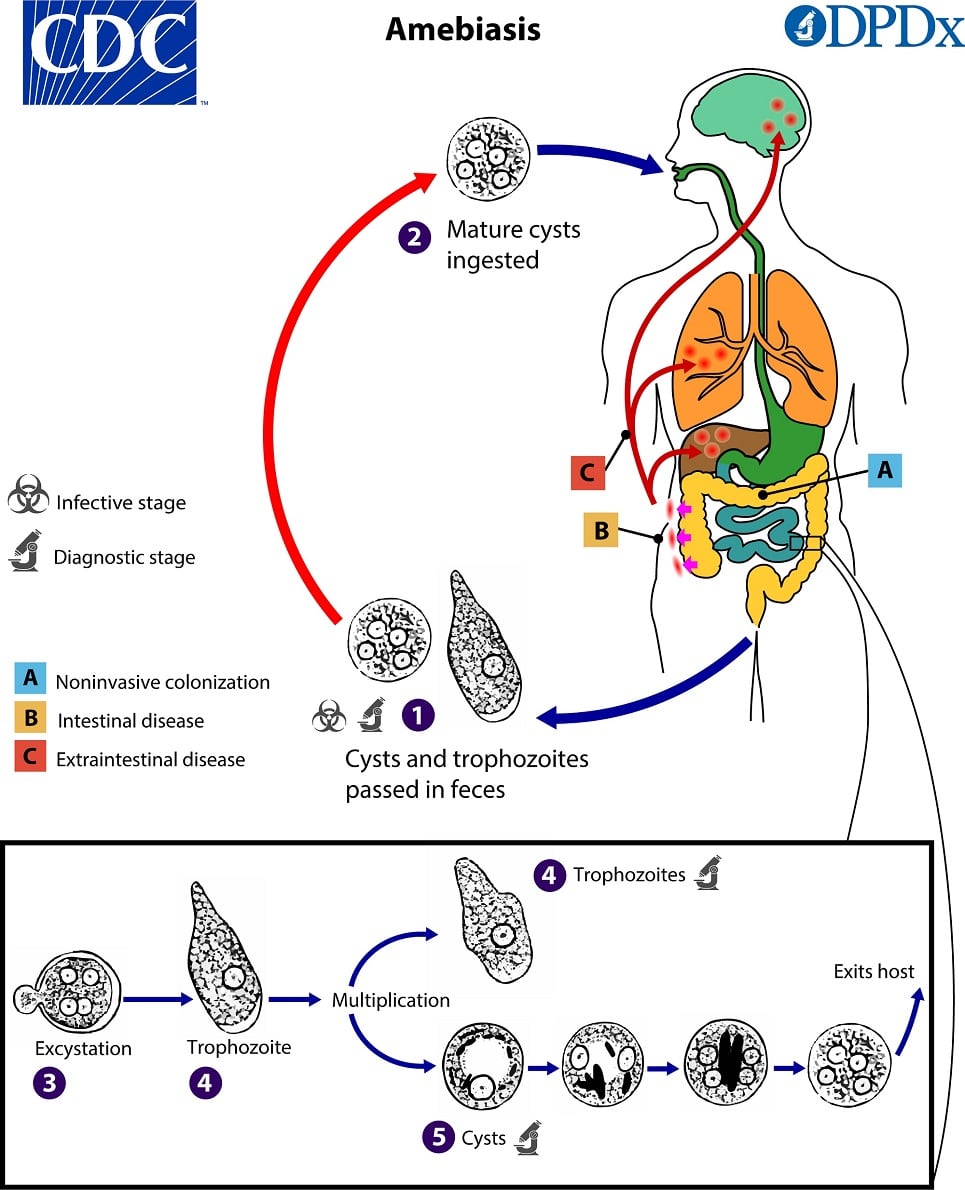
Pathogenesis: Infection with Entamoeba histolytica occurs when you ingest mature cysts in fecally contaminated food, water, or on hands. Excystation occurs in the small intestine, releasing trophozoites that migrate to the large intestine. In the colon, trophozoites multiply by binary fission and form cysts. Both stages are passed in feces.
Because cysts have a protective wall, they can survive for days to weeks in the external environment and are responsible for transmission. Trophozoites do not survive well outside the body and do not transmit infection.
Clinical features: Disease ranges from asymptomatic infection (“luminal amebiasis”) to invasive disease.
It causes flask-shaped intestinal ulcers. Intestinal amoebiasis typically presents with loose stools containing blood and mucus, along with abdominal pain and tenesmus. Pus from an amoebic liver abscess is thick and brownish, classically described as having an “anchovy sauce” appearance.
Laboratory diagnosis of amoebiasis: The intestinal form is diagnosed by identifying trophozoites or cysts in stool samples.
Amoebic antigen can be detected in stool by CIEP and ELISA. PCR and DNA hybridization can be used to detect E. histolytica DNA. For invasive amoebiasis, serologic tests for antibodies (CFT, CIEP, latex agglutination, ELISA, indirect immunofluorescence, and indirect haemagglutination) should be used.

Cyst of E. histolytica/E. dispar in a concentrated wet mount stained with iodine. Notice the chromatoid body with blunt, rounded ends (arrow).
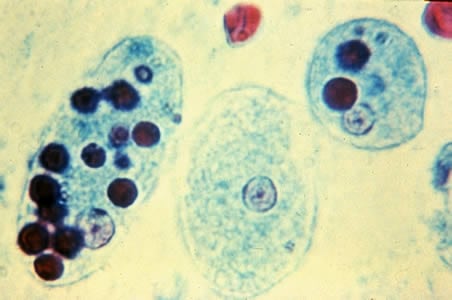
Trophozoites of E. histolytica with ingested erythrocytes stained with trichrome. The ingested erythrocytes appear as dark inclusions. The parasites above show nuclei that have the typical small, centrally located karyosome, and thin, uniform peripheral chromatin.
Sign up for free to take 1 quiz question on this topic