Six branchial (pharyngeal) arches form initially. Each arch is lined by ectoderm on the outside and endoderm on the inside. Somatic mesoderm and neural crest cells form the core of each arch. Neural crest cells develop into cartilage, bone, and connective tissue within the arch.
The ectoderm between adjacent arches forms the pharyngeal clefts. The endoderm between adjacent arches forms the pharyngeal pouches. Pharyngeal arch 5 involutes without forming any major structures, so the arches are numbered 1, 2, 3, 4, and 6. Each arch has an associated arterial (aortic) arch and a cranial nerve.
| Number | Artery | Nerve | Muscle | Neural crest derivatives |
|---|---|---|---|---|
| 1 (Mandibular) | Maxillary | Trigeminal (V) | Splits into maxillary and mandibular prominences. Mandibular gives rise to muscles of mastication, mylohyoid, anterior belly of digastric, tensor veli palatini and tensor tympani | Maxilla, zygomatic bone, squamous part of the temporal bone, palatine bone, vomer, mandible, Meckel’s cartilage, sphenomandibular ligament, incus and malleus |
| 2 (Hyoid) | Stapedial | Facial (VII) | Muscles of facial expression, posterior belly of digastric, stapedius, stylohyoid | Lesser horn of hyoid, upper half of body of hyoid bone, stapes, styloid process, stylohyoid ligament |
| 3 | Common carotid and internal carotid artery | Glossopharyngeal (IX) | Stylopharyngeus | Greater horn and lower half of body of hyoid bone |
| 4 | Arch of aorta, right subclavian artery | Superior laryngeal branch of the vagus nerve (X) | Cricothyroid and cricopharyngeus; muscles of soft palate except tensor veli palatini; muscles of pharynx except stylopharyngeus | Thyroid, cricoid, arytenoid, corniculate and cuneiform cartilages |
| 6 | Pulmonary arteries and ductus arteriosus | Recurrent laryngeal branch of Vagus nerve (X) | Skeletal muscles of the esophagus and intrinsic muscles of the larynx except for the cricothyroid | Thyroid, cricoid, arytenoid, corniculate and cuneiform cartilages |
| Number | Derivatives |
|---|---|
| 1 | Auditory tube and cavity of the middle ear |
| 2 | Crypts of palatine tonsil |
| 3 | Inferior parathyroid glands, thymus |
| 4 | Superior parathyroid glands, C cells, or parafollicular cells of the thyroid* |
| Number | Derivatives |
|---|---|
| 1 | External auditory meatus** |
| 2,3 and 4 | Obliterated |
*previously thought to arise from neural crest but now proved to be endodermal in origin.
** The first pharyngeal membrane between the ectoderm and endoderm of the first arch forms the tympanic membrane.
Preauricular cysts or fistulas arise from pharyngeal cleft 1. In contrast, remnants of clefts 2-4 present as cervical cysts or fistulas along the anterior border of the sternocleidomastoid muscle.
The thyroid gland develops from an endodermal thyroid diverticulum, which forms the follicles. It is connected to the tongue at the foramen caecum, located at the junction of the anterior ⅔ and posterior ⅓ of the tongue. The thyroglossal duct extends from the foramen caecum to the thyroid gland and is normally obliterated.
Ectopic thyroid tissue is typically located in the midline, anywhere from the base of the tongue to the lower neck, along the route taken by the thyroid during its migration from the tongue. The most common location is the lingual thyroid. High cervical, superior mediastinal, and paracardiac thyroids may be seen occasionally. It may cause hypothyroidism.
Both thyroglossal cyst and thyroglossal fistula occur in the midline. They form when the thyroglossal duct fails to obliterate fully. Infection is the most common complication. Definitive treatment is the Sistrunk procedure, in which the entire tract is removed along with part of the hyoid bone and the foramen caecum.
The anterior ⅔ of the tongue forms by fusion of the median and lateral tongue buds, which originate from the floor of the first pharyngeal arch. Occipital myoblasts invade the developing tongue and give rise to the intrinsic muscles of the tongue. The posterior ⅓ of the tongue develops from swellings arising from the floor of the third and fourth pharyngeal arches.
The face forms from the two mandibular prominences, two maxillary prominences, and the frontonasal prominence. These structures are derived from neural crest mesenchyme. Nasal pits divide the frontonasal process into two lateral nasal prominences and two medial nasal prominences.
The primary palate forms by fusion of the two medial nasal processes. The secondary palate forms by fusion of the palatine shelves, which grow from the maxillary processes.
Failure of the maxillary prominence on the affected side to join with the merged medial nasal prominences, resulting in a persistent labial groove
Failure of the maxillary prominences to merge with the medial nasal prominences
Very rare; caused by a mesodermal deficiency. Partial or complete failure of the medial nasal prominences to merge and form the intermaxillary segment.
Cleft lip is seen in Mohr’s syndrome (transmitted as an autosomal recessive trait).
It may be either unilateral or bilateral. It is often associated with cleft lip.
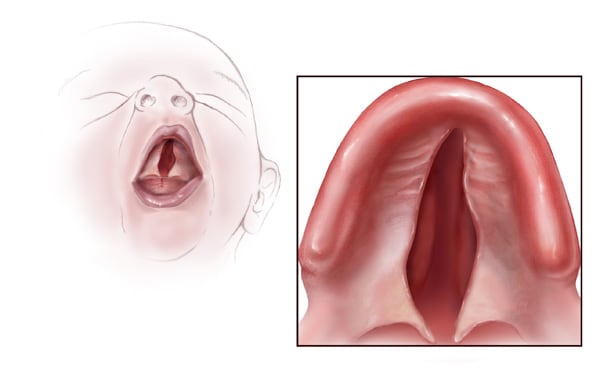
Occur anterior to the incisive foramen and are caused by a failure of the lateral palatine processes to meet and fuse with the primary palate
Involve both the primary and secondary palate and are caused by failure of the lateral palatine processes to meet and fuse with each other, the primary palate, and the nasal septum
These clefts are posterior to the incisive foramen and are caused by a failure of the lateral palatine processes to meet and fuse with each other and the nasal septum.
Sign up for free to take 4 quiz questions on this topic