The respiratory system is divided into a conducting zone and a respiratory zone. Only the respiratory zone participates in gas exchange.
The nasal septum divides the nasal cavity into right and left halves.
The lateral nasal wall has three bony projections called the superior, middle, and inferior conchae. These form the three turbinates and border spaces called meatuses (superior, middle, and inferior).
The nasal mucosa is ciliated, pseudostratified columnar epithelium. It produces IgA and IgE.
The nose has a rich blood supply from branches of the external and internal carotid arteries. The external nose is supplied by the facial artery, infraorbital artery, and ophthalmic artery.
Kiesselbach’s plexus (Little’s area) is on the anterior and inferior part of the nasal septum. It is the site of anastomoses between four major arteries:
It is the major site of epistaxis (bleeding from the nose).
Posterior bleeding derives primarily from the posterior septal nasal artery (a branch of the sphenopalatine artery), which forms part of the Woodruff plexus. The Woodruff plexus is located on the lateral nasal wall, posterior to the inferior turbinate, and is mainly a venous plexus. Posterior nosebleeds are more difficult to control and can lead to aspiration.
The pharynx is a common passage for the alimentary and respiratory tracts. It is divided into the nasopharynx, oropharynx, and laryngopharynx.
The pharynx receives the auditory (eustachian) tube, which connects it to the middle ear. Infections can spread from the pharynx to the middle ear through this route.
The nasopharynx also contains the nasopharyngeal tonsils (adenoids) on the posterior wall. The adenoid tonsil is supplied by the ascending palatine branch of the facial artery, ascending pharyngeal artery, pharyngeal branch of the internal maxillary artery, artery of the pterygoid canal, and the ascending cervical branch of the thyrocervical trunk.
The oropharynx extends from the nasopharynx to the epiglottis. It contains a lymphatic ring of nasopharyngeal, tubal, palatine, and lingual tonsils. The palatine tonsil is supplied by the tonsillar and ascending palatine branches of the facial artery, the ascending pharyngeal artery, the dorsal lingual branch of the lingual artery, and the palatine branch of the maxillary artery.
The laryngopharynx ends at the cricoid cartilage.
The wall of the pharynx has an external circular and an internal longitudinal layer of muscles.
The larynx extends from the C3 to C6 vertebrae.
The larynx has three single and three paired cartilages: thyroid, cricoid, epiglottic, arytenoid, corniculate, and cuneiform cartilages.
The thyroid cartilage is superficial and can be seen and palpated as the “Adam’s apple”. The cricoid cartilage is at the level of the C6 vertebra.
In cricothyrotomy, the cricothyroid membrane is incised to access the larynx in an emergency to establish patency of the airway when endotracheal intubation is not possible.
The trachea begins at the lower edge of the cricoid cartilage and ends at the level of the T4 vertebra and sternal angle, at the carina, where it divides into the right and left main bronchi.
The trachea is located anterior to the esophagus. It is incompletely surrounded on the anterior and lateral sides by about 15-20 C-shaped hyaline cartilages. These provide flexibility and help keep the trachea open, preventing airway collapse.
The trachealis muscle (smooth muscle) runs along the posterior wall. The posterior wall is devoid of cartilage, allowing the esophagus (posterior to the trachea) to expand during swallowing.
The trachea is lined by respiratory epithelium: ciliated, pseudostratified columnar epithelium with goblet cells. The mucosal lining also contains:
The lobes of the thyroid gland are anterolateral to the cervical trachea, and the thyroid isthmus crosses the trachea anteriorly at the level of the second or third tracheal rings.
There are two main bronchi.
The main bronchi divide into lobar bronchi.
The lobar bronchi divide into segmental bronchi, which supply the bronchopulmonary segments.
The bronchi are lined by respiratory epithelium, as described above. They have a prominent layer of circular smooth muscle. Hyaline cartilages are present in the wall.
The bronchioles are lined by simple ciliated columnar epithelium with goblet cells and Clara cells.
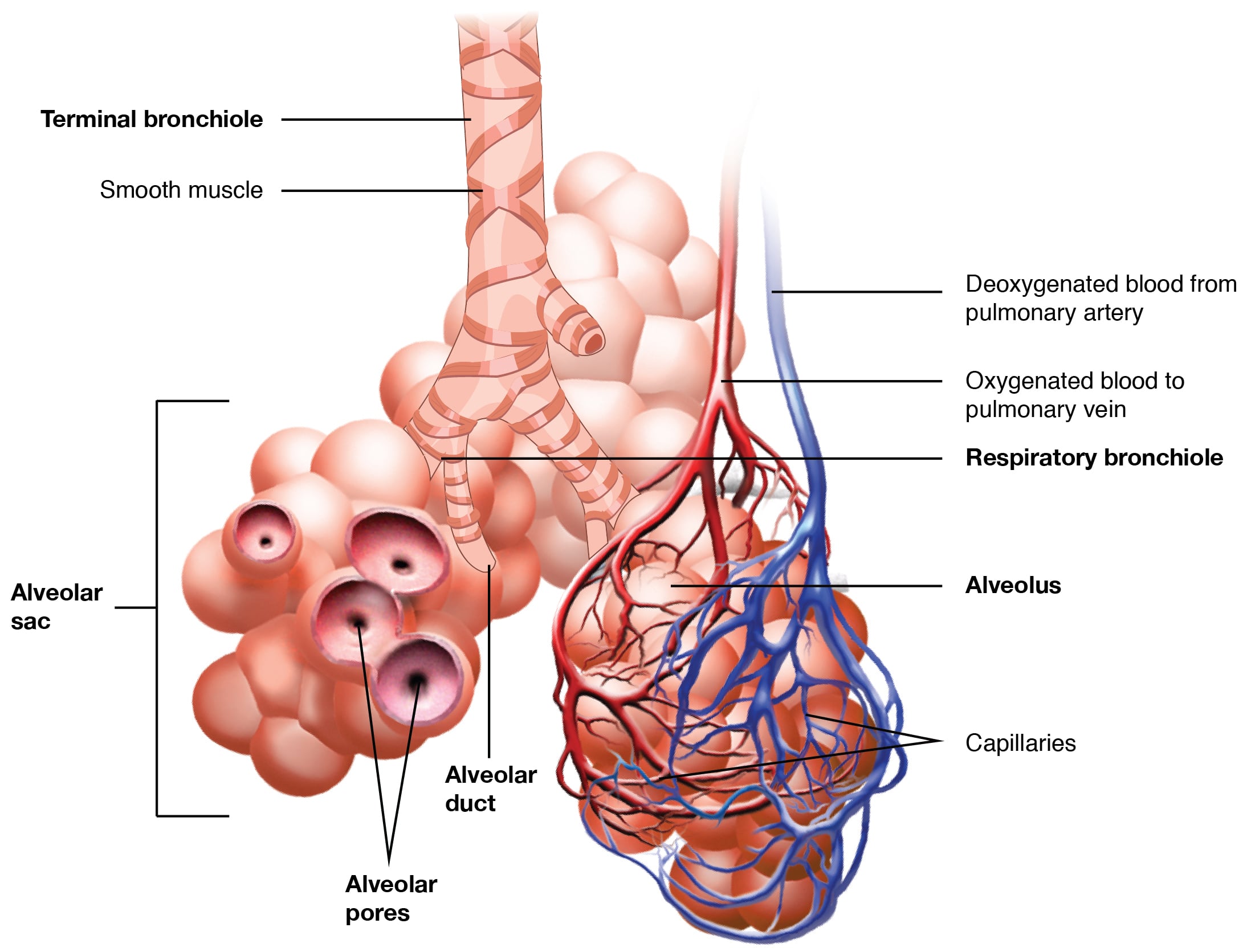
The terminal and respiratory bronchioles are lined by simple, ciliated, cuboidal epithelium with Clara cells. Cartilage is absent in the respiratory bronchioles. Occasional alveoli open into the terminal and respiratory bronchioles.
Alveolar ducts are tubular structures lined by simple squamous epithelium. The alveolar ducts are lined by alveoli. Cilia are absent in the epithelium of the alveolar ducts and alveoli.
Alveolar ducts connect to alveolar sacs, which give rise to clusters of alveoli. A network of capillaries surrounds the alveoli.
The alveolar lining is made mainly of two types of cells: type I and type II pneumocytes.
Alveolar macrophages are present in the septae.
Pores of Kohn are present in the interalveolar septum. Their role is collateral ventilation and equalization of pressure across the alveoli. They also form channels for the spread of infections like pneumonia and in cancers.
Sometimes, alveolar brush cells are called type III pneumocytes. Their role is ill defined.
The blood air barrier is formed by the surfactant layer, type I pneumocyte, basement membrane, and capillary endothelial cell. Diffusion occurs across the blood air barrier.
Both lungs are divided into lobes by fissures: 3 on the right and 2 on the left.
The right lung is further divided into 10 segments:
The left lung has 8 segments:
Aspiration pneumonia occurs in the apical segment of the lower lobes (right more common) and the posterior segment of the upper lobes in a supine patient. In the erect position, aspiration pneumonia occurs in the basal segment of the lower lobe (right more common).
Surface anatomy is important for assessing thoracic and abdominal injuries and for procedures like thoracotomy.
The apices of the lungs extend 3 cm above the medial third of the clavicle.
The inferior margins of the lung are at:
The parietal pleura is situated about two vertebral levels lower than the lung margins.
The upper lobe of the right lung extends up to the fourth rib, the middle lobe extends from the fourth to sixth ribs, and the lower lobe is below the sixth rib. On the left, the upper lobe extends to the sixth rib, and the lower lobe is below it.
Sign up for free to take 9 quiz questions on this topic