The sciatic nerve is the largest nerve in the human body. It arises from the ventral rami of spinal nerves L4-S3 (lumbosacral plexus). It travels posteriorly in the lower limb, continuing down toward the heel. Near the popliteal fossa, it divides into the tibial nerve and the common peroneal (fibular) nerve.
| Nerve | Muscles supplied | Actions | Sensory supply* |
|---|---|---|---|
| Sciatic Nerve** | Biceps femoris, semimembranosus, semitendinosus, ischial part of the adductor magnus (hamstrings) | Flexion of the knee and adduction of the hip | No direct sensory innervation |
| Tibial Nerve | Gastrocnemius, soleus, plantaris and popliteus, flexor hallucis longus, flexor digitorum longus, tibialis posterior | Plantar flexion and flexion of the toes | As medial and lateral plantar nerves to the sole of foot and heel |
| Common Peroneal Nerve | Tibialis anterior, extensor hallucis longus, extensor digitorum longus, peroneus longus, brevis and tertius | Dorsiflexion of the foot, toe extension and eversion of the foot | As superficial peroneal nerve to the posterolateral part of leg and dorsum of the foot. As deep peroneal nerve to skin between first and second toes |
** The posterior cutaneous nerve of thigh runs with the sciatic nerve and supplies sensory innervation to the posterior thigh and inferior buttocks. The sural nerve is formed by contributions from tibial and common peroneal nerves and is sensory to the calf and a small area along the lateral foot.
Sciatica is low back pain associated with radiating pain down the buttocks and posterior lower limb in the distribution of the sciatic nerve. The pain is typically shooting or burning, varies in intensity, and may be accompanied by muscle weakness and numbness.
Any condition that impinges on or irritates the sciatic nerve can cause sciatica, for example:
Acute compartment syndrome occurs when intracompartmental pressure increases enough to interfere with local circulation. It can occur anywhere a compartment is present (e.g., arm, forearm, hand, abdomen, lower limbs).
Common causes include:
Clinical features include local pain out of proportion to the injury (often worse with passive stretching), numbness, possibly absent pulses, and local edema and swelling. Treatment is early decompression with fasciotomy.
Tarsal tunnel syndrome is caused by compression of the tibial nerve or its branches as it passes through the tarsal tunnel under the flexor retinaculum at the ankle. It presents with pain, tingling, and numbness radiating from the ankle medially into the ankle and foot.
Common peroneal nerve injury causes foot drop and sensory loss in the peroneal nerve distribution. Injury is common because the nerve lies close to the skin on the lateral part of the leg, just under the knee, as it winds around the neck of the fibula.
It can occur with:
Deep tendon reflexes are stretch reflexes modulated by muscle spindles. Reflexes are graded from 0 to 4+:
| Reflex | Nerve Root |
|---|---|
| Jaw jerk | Trigeminal nerve |
| Biceps jerk | C5,6 |
| Triceps jerk | C6,7 |
| Brachioradialis | C5,6 |
| Finger jerk | C8-T1 |
| Knee jerk | L3,4 |
| Ankle jerk | S1 |
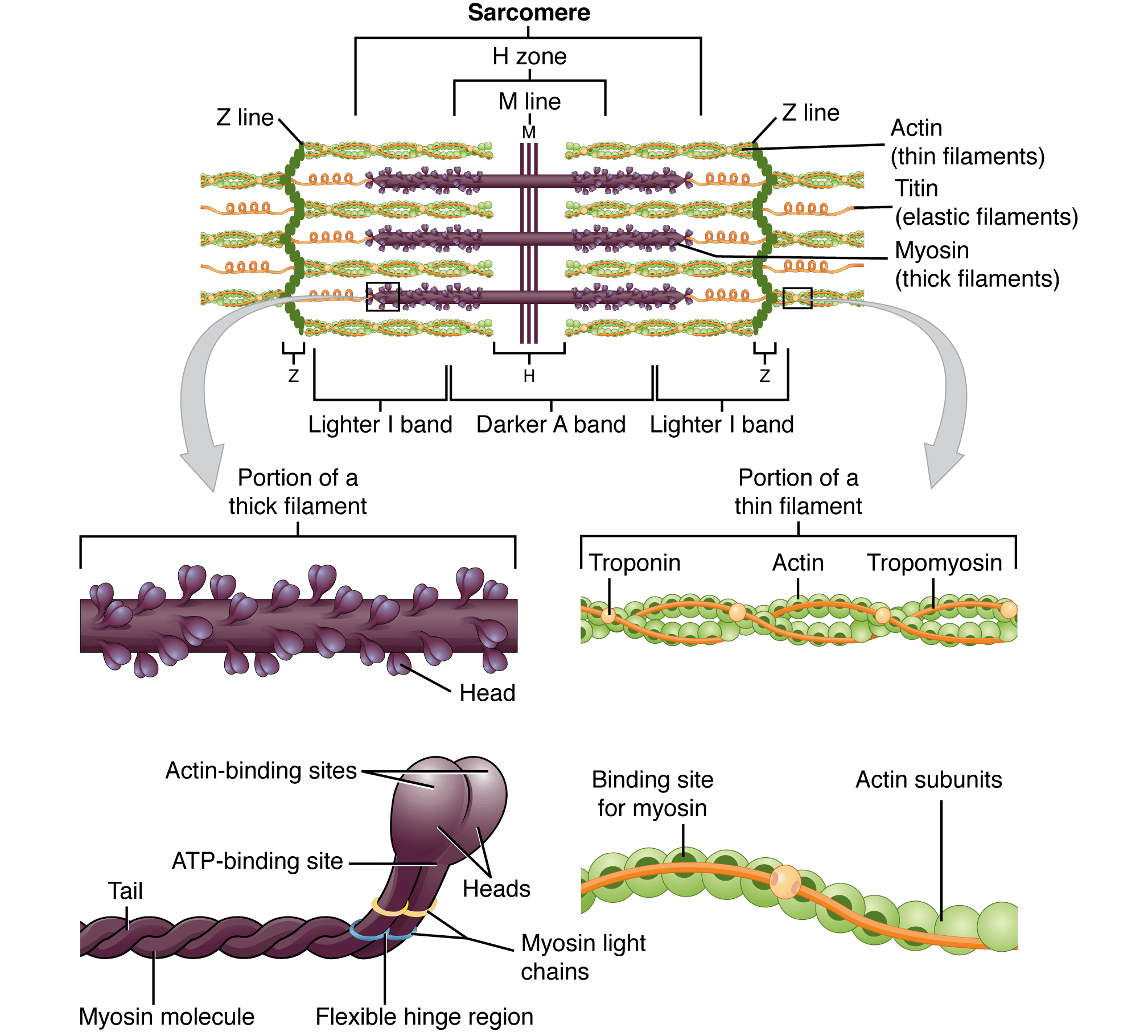
The sarcomere is the basic functional unit of muscle. Sarcomeres join end-to-end to form muscle fibers, which are covered by endomysium. Muscle fibers bundle together to form fascicles, which are covered by perimysium. Fascicles are then covered by epimysium.
Each sarcomere is bounded by Z discs. Thin actin filaments attach to the Z discs.
During muscle contraction:
According to the sliding filament theory of muscle contraction, myosin binds to actin and functions as a motor that drives filament sliding. This process requires energy in the form of ATP.
Sign up for free to take 2 quiz questions on this topic