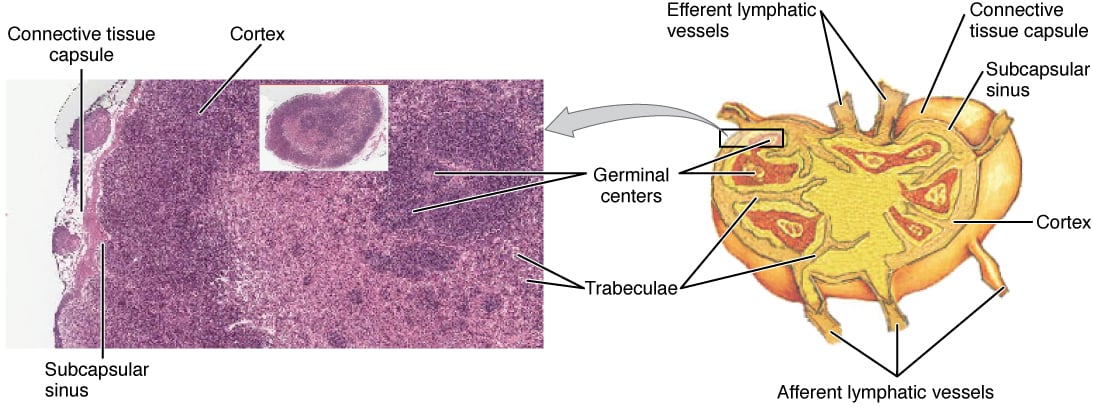
Lymph nodes are small, bean-shaped glands located along lymphatic vessels. They act as drainage and processing sites for lymph components. Each node is surrounded by a tough capsule that extends inward as trabeculae, dividing the lymph node into compartments. Structurally, a lymph node has an outer cortex and an inner medulla. It receives lymph through afferent lymphatics, and lymph leaves through efferent lymphatics.
The cortex has an outer and an inner zone.
The outer cortical zone consists of follicles made of mature B cells. The center of a follicle is the germinal center, which contains actively dividing B cells and plasma cells. Follicular dendritic cells are present in the cortex and play an important role in antigen presentation.
The inner cortical zone is also called the paracortex (the thymus-dependent zone). It mainly contains mature T cells.
The medulla contains medullary cords of B cells and plasma cells. The medulla is the major site of antibody production. Macrophages are abundant here and perform phagocytosis as part of the body’s defense system.
[Think of lymphatics as police patrols and lymph nodes as a “detention facility.”]
Reticular cells (fibroblasts) are present throughout the lymph node. Their primary function is to lay down reticular fibers and type III collagen, providing structural support for the node.
The efferent lymphatics and blood vessels leave the lymph node at the hilum.
The spleen is a major secondary lymphoid organ. Knowing its surface anatomy helps with abdominal trauma questions.
The spleen is located in the left hypochondrium and partly in the epigastrium. It extends from ribs 9 to 11, with its medial end located 5 cm from the midline.
A healthy spleen is not palpable in adults. In splenomegaly, the spleen weighs more than 500 grams or has a span (from one end to the other) of more than 11 cm.
It should be less than 10 cm in kids at 8 years and less than 6 cm at 3 months. In age groups between 3 months and 8 years, splenic size will range from 6 - 8 cm. At and above the age of 10, refer to adult size ranges. A palpable spleen is found in most premature infants and 30% of term infants. A spleen tip is still palpable in 10% of infants at 1 year of age and in 1% of children at 10 years of age.
Normal spleens are soft at the midclavicular line, nontender, and often palpable only on deep inspiration. Dullness on percussion beyond the 11th intercostal space suggests splenomegaly.
A spleen edge palpated >2 cm below the costal margin is always an abnormal finding.
Splenic tenderness is always abnormal.
The spleen is a capsulated organ. The capsule extends into the splenic pulp as trabeculae. Splenic tissue is divided into red pulp, white pulp, and a marginal zone in between.
White pulp looks pale on gross appearance and consists of follicles and the periarteriolar lymphatic sheath (PALS). The follicles are closely associated with the central arteriole and consist of mature B cells and a germinal center of dividing B cells. The PALS comprises mature T cells arranged as a sheath around the central artery.
Marginal zone comprises macrophages and antigen presenting cells like dendritic cells.
Red pulp consists mostly of RBCs. It is arranged as cords of Billroth separated by venous sinusoids. Cords of Billroth are made of RBCs, macrophages, plasma cells, and lymphocytes. Senescent and abnormal RBCs are broken down in the red pulp by splenic macrophages.
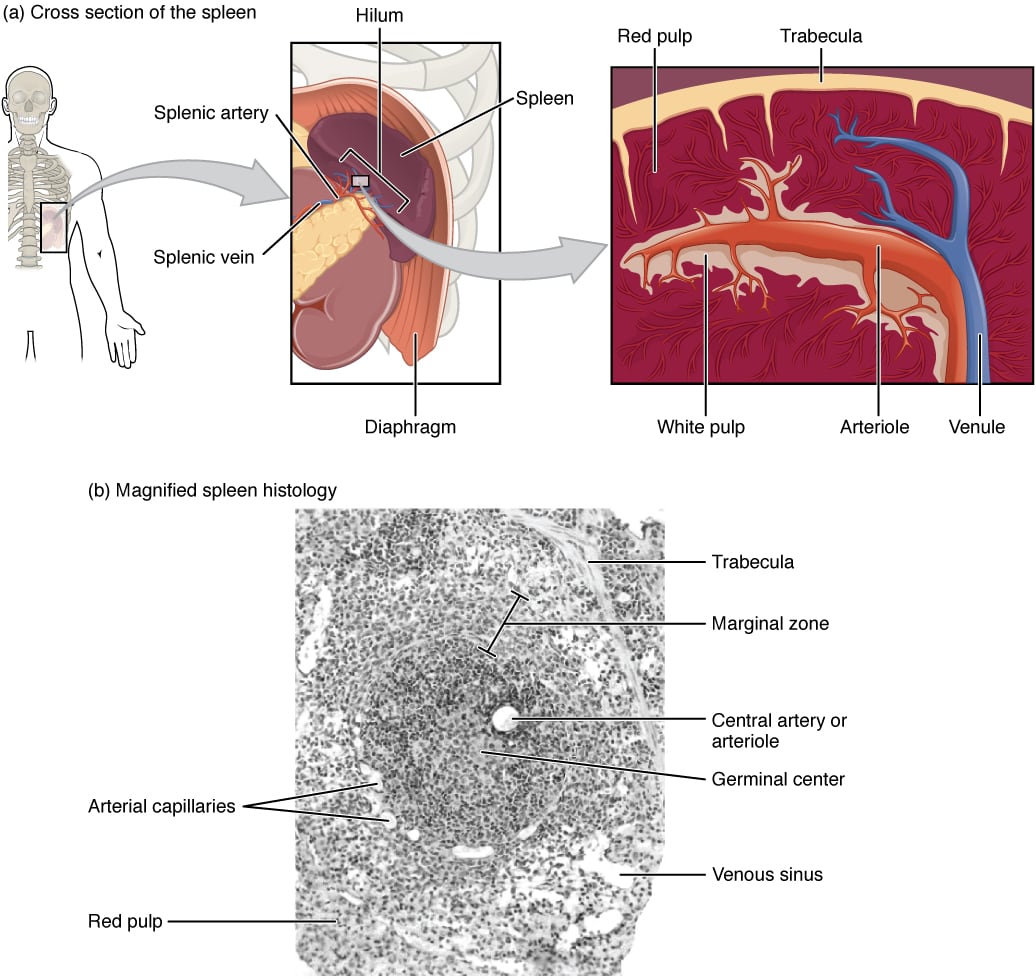
The spleen is attached to the stomach. (b) A micrograph of spleen tissue shows the germinal center. The marginal zone is the region between the red pulp and white pulp, which sequesters particulate antigens from the circulation and presents these antigens to lymphocytes in the white pulp. EM × 660.
The thymus is an encapsulated, bilobed gland in the superior mediastinum behind the sternum, extending into the anterior mediastinum. It is the site of T cell maturation. With age, the thymus undergoes involution and is replaced, in part, by adipose tissue.
The thymus is divided into an outer cortex and an inner medulla.
The cortex contains thymocytes (T stem cells, pre T cells, and immature T cells) and thymic epitheliocytes. Thymic epitheliocytes provide structural support and secrete thymotaxin, thymosin, and thymopoietin, which are involved in T cell maturation. Thymic epitheliocytes are also called “thymic nurse cells” because they essentially “nurse” immature T cells to maturation.
The medulla contains mature T cells, including CD4+ (helper) T cells, CD8+ (cytotoxic) T cells, and suppressor T cells. It also contains thymic epitheliocytes and Hassall’s corpuscles.
In some infants, the thymus may appear as a triangular extension lateral to the mediastinum called a “thymic sail sign” (like the sail of a ship).
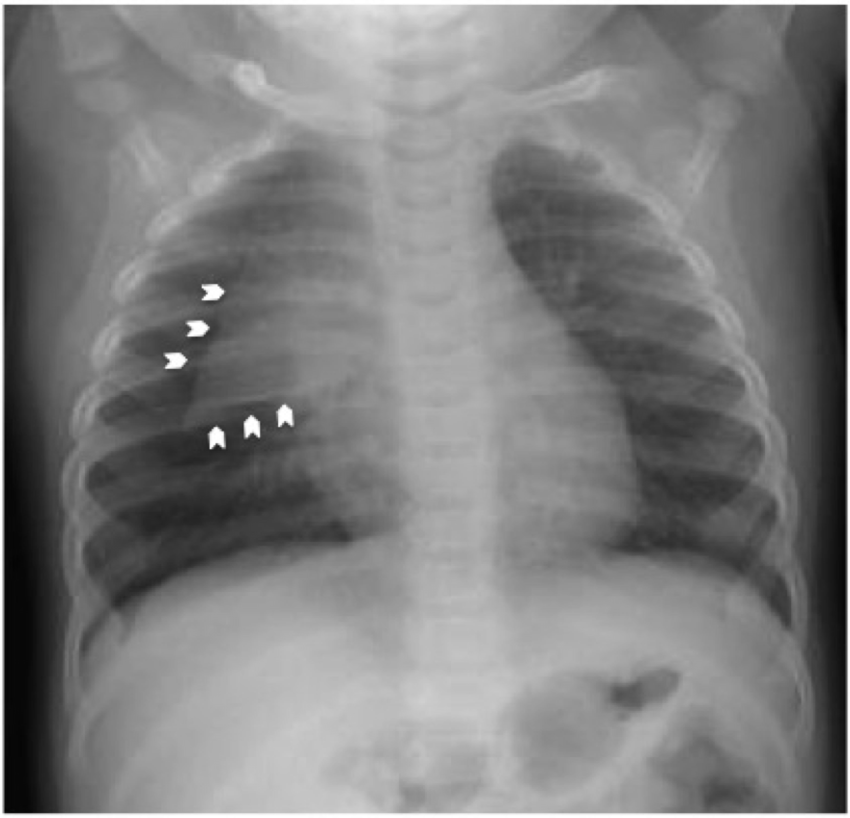
“Sail sign” on thymus x-ray
Hassall’s corpuscles are whorl-like collections of thymic epithelial cells, macrophages, interdigitating dendritic cells, myoid cells, and occasionally, mast cells and lymphocytes. They are involved in the removal of apoptotic thymocytes and the maturation of developing thymocytes. They play a vital role in the generation of regulatory T cells and the regulation of lymphopoiesis.

MALT contains roughly half of the lymphocytes of the immune system. It is located along mucosal surfaces, including the gastrointestinal tract (GALT or gut-associated), nasopharynx, bronchus, larynx, salivary glands, and conjunctiva.
MALT secretes IgA and mediates mainly a TH2 type immune response. It is also associated with developing immune tolerance to antigens exposed to the mucosa.
Intraepithelial lymphocytes are another component of MALT. These are T lymphocytes found among epithelial cells of mucosal tissues.
M cells are specialized epithelial cells associated with MALT tissues. They transport microorganisms and molecules from the intestinal lumen to MALT follicles. M cells lack microvilli and have tight cell junctions. They act like antigen presenting cells.
Peyer’s patches are GALT present in the mucosa and submucosa along the antimesenteric border, most abundant in the ileum.
Immune responses in MALT are initiated locally at inductive sites, and activated lymphocytes then migrate distally to effector sites.
Sign up for free to take 16 quiz questions on this topic