Lymphomas are malignancies that arise in lymph nodes and other lymphoid tissues. They’re broadly divided into Hodgkin’s lymphoma (HD) and non-Hodgkin’s lymphomas (NHL).
| Type | Features |
| Diffuse large B cell lymphoma | Most common NHL. Commonly seen in the chest, neck, armpit, and abdomen. Associated with HIV and EBV. Shows diffuse sheets of large malignant lymphoid cells. |
| Follicular lymphoma | Associated with t(14;18) and overexpression of anti-apoptotic bcl2. More common in adults. Appears as malignant follicles, typically with lack of a mantle zone, uniformly filled with malignant lymphoid cells and loss of normal lymph node architecture. Presents with generalized painless lymphadenopathy. |
| Cutaneous T cell lymphoma | Involves the skin. Presents as rash, plaques, and dry, itchy, eczema-like lesions; may also cause lymphadenopathy and hepatosplenomegaly. Mycosis fungoides shows infiltration of skin by malignant T cells with cerebriform nuclei (Sezary cells) and intraepidermal collections of atypical cells called Pautrier’s microabscesses. Sezary syndrome occurs when malignant T cells (Sezary cells) invade the bloodstream. |
| Small cell lymphocytic lymphoma | Counterpart of CLL in lymph nodes. Shows pseudo-follicles of mature-looking malignant lymphoid cells and smudge cells. B-cell origin. Autoantibodies to RBCs and platelets may be seen, along with hypogammaglobulinemia and monoclonal Ig spikes. May involve bone marrow. |
| Nodal marginal zone lymphoma | Arises from B cells. Seen in older persons with HCV. Presents with lymphadenopathy and B symptoms. |
| Mucosa associated lymphoid tissue lymphoma or MALTomas or extranodal marginal zone lymphomas | Arises in MALT tissues of the GIT, respiratory tracts, thyroid, etc. Associated with H.pylori. |
| Anaplastic large cell lymphoma | More common in young adults and children. Ki 1 or CD30+. Presents with lymphadenopathy; bone marrow and CNS involvement may occur. Malignant cells are cytotoxic T cells. Shows anaplastic large cells with horseshoe nuclei and nuclear inclusions (doughnut cells). |
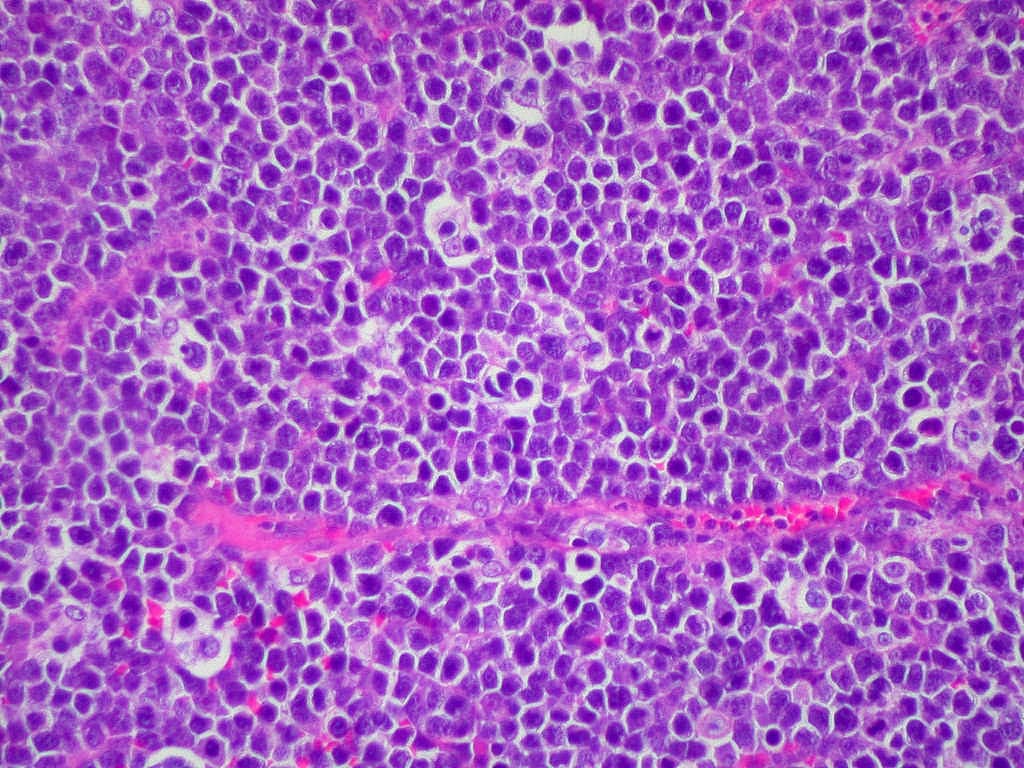
| Burkitt’s lymphoma | Associated with EBV infections and t(8;14). Has endemic and sporadic forms. Shows a “starry sky” appearance with diffuse blue lymphocytes with scant cytoplasm interspersed with tingible-body macrophages*; Ki-67 positive. Can progress to leukemia. Jaw and GI tract lesions are more common. |
| CNS lymphoma | May be primary or secondary; may also involve eyes, spinal cord, and meninges. Most are diffuse large B-cell lymphomas. Associated with AIDS and immunosuppression. Presents with headache, nausea, vomiting, seizures, double vision, hearing loss, and arm or leg weakness. |
| T-Lymphoblastic lymphoma/leukemia | Rare; mostly seen in teens and young adults. Considered either lymphoma or ALL depending on bone marrow involvement. Origin is thymus. Presents as a mediastinal mass with dyspnea and swollen face and arms. Mature-looking T cells on histology. |
| Mantle cell lymphoma | Develops from the mantle zone of lymph nodes. B-cell origin. Presents with lymphadenopathy and GIT involvement. Associated with overexpression of cyclin D1 and t(11;14). Seen in older males. |
| Adult T cell leukemia/lymphoma | More common in Japan, the Caribbean, and Africa. Associated with HTLV-1. Seen in adults. May present acutely or chronically. Skin, liver, lung, and lymph node involvement may occur. Hypercalcemia and immunocompromise can occur. Histology shows “flower cells,” which are malignant lymphocytes with a convoluted nucleus. |
*tingible-body macrophages are histiocytes phagocytosing apoptotic bodies.
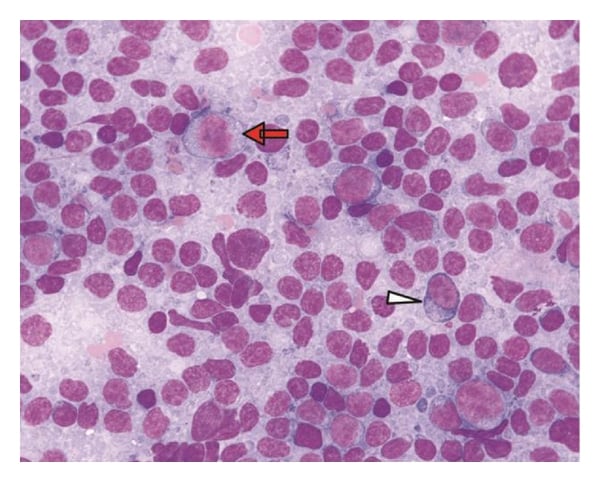
Monocytoid B-cells (red arrow) and plasmacytoid cells (white arrowheads) are often found in marginal zone lymphoma
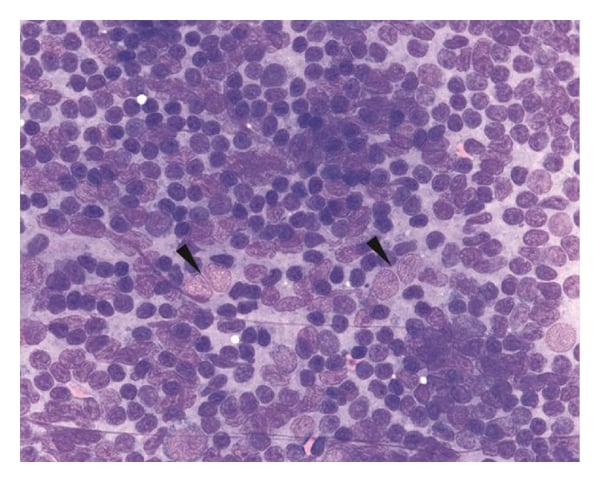
Follicular dendritic cells are a prominent feature of follicle center fragments present in samples of follicular lymphoma.
The CHOP regimen (cyclophosphamide, doxorubicin [hydroxydaunorubicin], vincristine, and prednisone) is used to treat NHL. Other treatments include rituximab, intrathecal methotrexate, CAR -T cell immunotherapy, stem cell transplantation, and radiotherapy. Hyper-CVAD, CODOX-M, and EPOCH are chemotherapy regimens used for Burkitt’s lymphoma.
| Classic Hodgkin’s disease | |
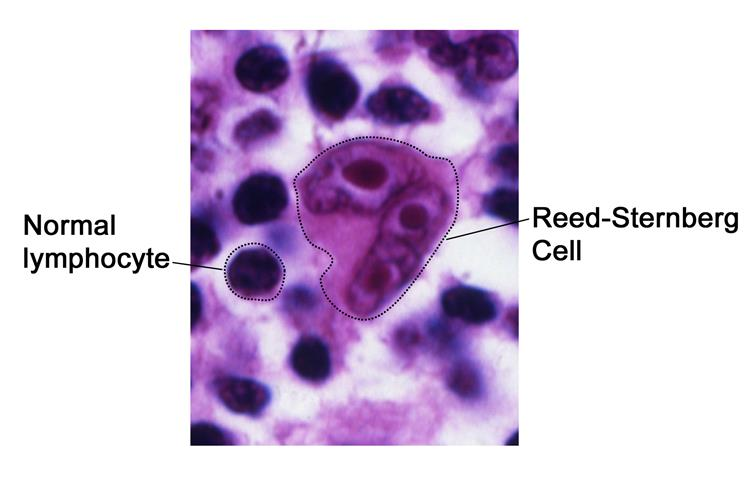
| Nodular sclerosis | Most common. Nodular pattern with fibrotic bands; lacunar type Reed-Sternberg cells are seen. |
| Mixed cellularity | Diffuse pattern with a mixed infiltrate; classic Reed-Sternberg cells are seen. Common sites are the abdomen and spleen. Associated with HIV. |
| Lymphocyte predominant | Better prognosis. Prominent lymphocytic infiltrate. |
| Lymphocyte depletion | Bad prognosis. Associated with HIV and EBV. Diffuse pattern with many Reed-Sternberg cells and fewer lymphocytes. |
| Nodular lymphocyte predominant | |
| Less common and slow growing compared to classic HD. Reed-Sternberg cells are absent or few. Lymphocytic and histiocytic (LH) or “popcorn cells” are seen on histology. CD20+, CD15+ and CD30+. Associated with HLA-DRB1 and HLA-DQB1. | |
Hodgkin’s disease presents with lymphadenopathy (commonly in the axilla, chest, groin, and abdomen), B symptoms, and hepatosplenomegaly. The age distribution of HD is bimodal, occurring more frequently in the 15-35 and >60 year age groups.
Chemotherapy regimens include:
Stem cell transplantation and radiotherapy can also be used.
Nodular lymphocyte predominant HD is treated by local excision, radiotherapy, or close observation. Rituximab plus chemotherapy like CHOP can be used for advanced disease.
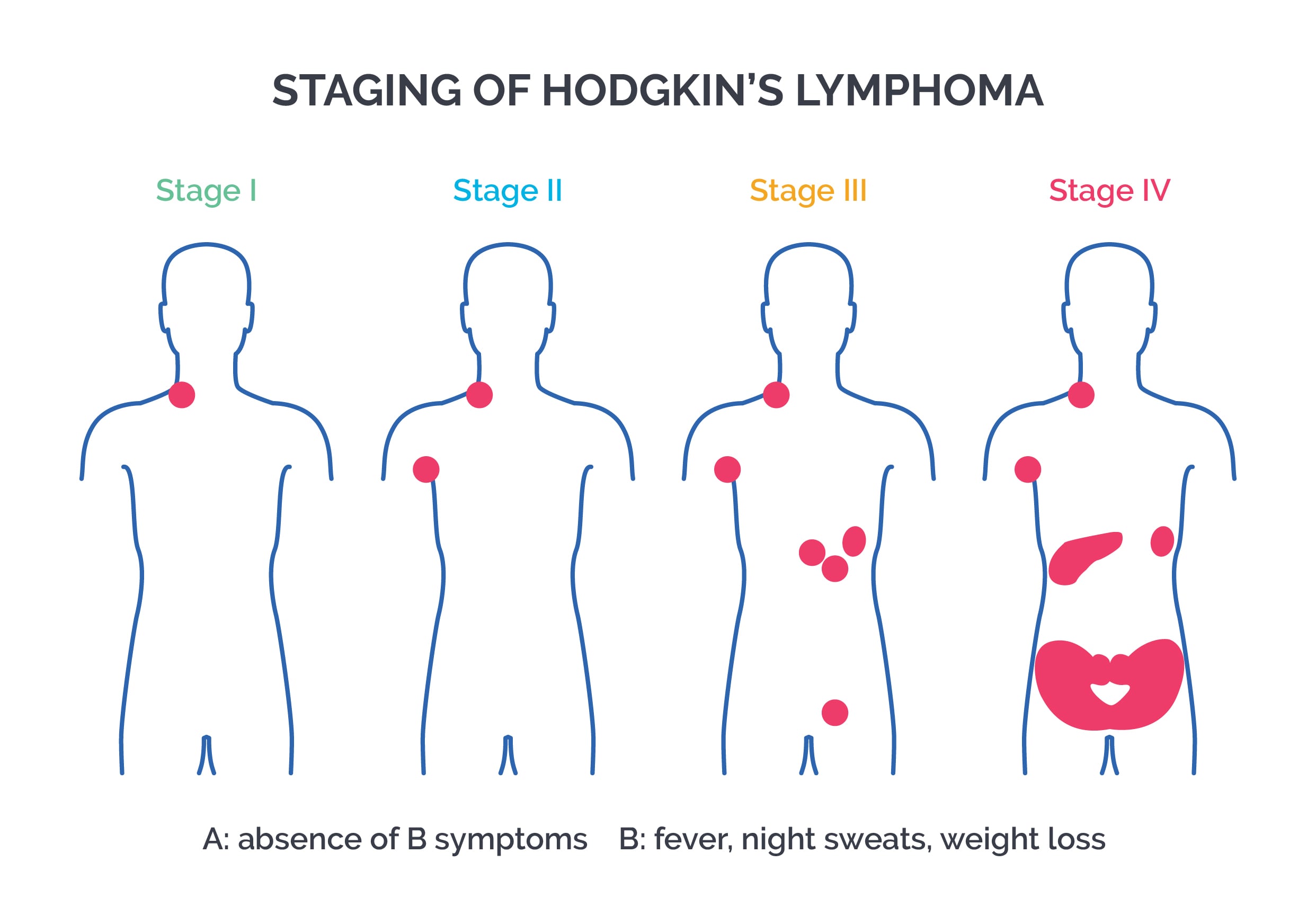
Staging of Hodgkin’s disease: Staging involves a combination of symptoms plus imaging techniques like CT scan. Ann Arbor classification is used for staging. Spleen and thymus are included as lymphatic areas.
Stage I: A single lymph node area or single extranodal site
Stage II: Two or more lymph node areas on the same side of the diaphragm
Stage III: Lymph node areas on both sides of the diaphragm
Stage IV: Disseminated disease or involvement of multiple extranodal organs, liver, or bone marrow involvement
A: Absence of B symptoms
B: Presence of B symptoms
Suffix S: Splenic involvement
Sign up for free to take 4 quiz questions on this topic