It’s an inherited disease characterized by crescent-shaped (sickled) RBCs. Sickled cells are removed by the spleen, causing anemia. They can also occlude the microcirculation, leading to tissue ischemia and infarction.
The underlying abnormality is an atypical hemoglobin called HbS. Under deoxygenated conditions, HbS becomes relatively insoluble and forms aggregates (polymers) with other hemoglobin molecules inside the RBC. HbS is produced by mutations in the HBB gene, which normally codes for the beta globin chain of hemoglobin. The disease-causing mutation is a point mutation in the HBB gene (chromosome 11) that results in a single amino acid substitution (valine for glutamic acid) at the 6th position in the β globin chain.
Patients with HbSS are less susceptible to P. falciparum malaria. The disease is more common in the African American population.
RBCs in SCA also appear to have increased binding affinity for vascular endothelium. Intimal hyperplasia is also seen. These factors, along with RBC sickling, put patients at risk of vaso-occlusive crises.
In young children, vaso-occlusive crises most commonly manifest as dactylitis, a painful swelling of the hands, fingers, feet, and toes. Osteomyelitis, osteonecrosis, splenic infarct, splenic sequestration, acute chest syndrome, stroke, papillary necrosis, and renal insufficiency can also occur in SCA.
Pulmonary complications are the leading cause of death in SCA. Pneumonia in SCA is most commonly caused by Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Chlamydia pneumoniae, and Salmonella organisms.
Acute chest syndrome: This is a complication of SCA that can be precipitated by bacterial pneumonias, pulmonary vascular occlusion, fat embolism from bone infarcts, opioid use, Parvovirus B19, and general anesthesia. Any of these factors may cause local deoxygenation and precipitate a crisis. It presents acutely with fever, chest pain, cough, dyspnea, tachypnea, and respiratory distress syndrome. It is more common in children with SCA. CxR shows single or multiple areas of pulmonary consolidation. Treatment consists of hydration, transfusion, supplemental oxygen, and analgesia. Supportive measures such as antibiotics, steroids, and mechanical ventilation may be needed.
Pain crises: These present as acute and recurrent episodes of mild to severe pain, often near the joints, chest, back, abdomen, and upper and lower limbs. They are caused by vaso-occlusion leading to ischemia. Dehydration, extremes of temperature, exposure to low atmospheric oxygen (such as high altitude), infections, and strenuous exercise can precipitate pain crises. Management includes adequate pain relief (including opioids if needed), hydroxyurea, intravenous fluids, oxygen, and blood transfusion.
Skeletal complications: A “hair on end” appearance of the skull is seen due to medullary expansion and widening of the diploic space. Increased bone marrow cellularity predisposes to bone hypoxia, infarction, and osteomyelitis. Repeated infarctions cause osteonecrosis. A “Lincoln log” or “H-shaped” vertebral deformity is seen.
Dactylitis (hand-foot syndrome) is often the first clinical manifestation of SCA. It presents with fever and painful, swollen hands and feet and is most commonly seen in children younger than 4 years of age. It is caused by bone infarction along with subperiosteal new bone formation. X-ray shows a “moth-eaten” appearance of the bones.
Osteomyelitis is seen in the diaphysis of long bones such as the femur, tibia, and humerus in SCA. It presents with pain, fever, and erythema. The most commonly encountered organism is Salmonella (especially the nontypical serotypes S typhimurium, S enteritidis, S choleraesuis, and S paratyphi B), followed by S aureus.
Splenic complications: Patients with SCA undergo autosplenectomy due to recurrent infarctions. The spleen becomes fibrotic and calcified, and this may occur by early childhood. Loss of splenic function makes patients prone to infection with S pneumoniae, H influenzae type B, and Salmonella, Klebsiella, and other encapsulated bacteria. Penicillin prophylaxis is required, as well as pneumococcal and H. influenzae vaccines.
Splenic sequestration syndrome is a feared and potentially fatal complication. It is characterized by rapid pooling of blood within the spleen, intravascular volume depletion, rapid reduction in Hb and hematocrit, left upper quadrant pain, abdominal fullness, splenomegaly, and cardiovascular collapse. Splenic sequestration is triggered by antecedent viral infections, pain crises, or bacteremia and is more common in young children. It is managed with blood transfusions and splenectomy if recurrent.
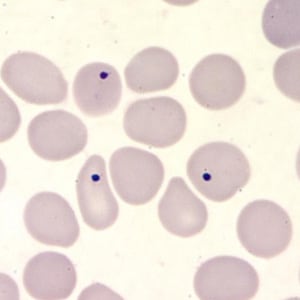
Howell-Jolly bodies in a thin blood smear, stained with Giemsa. Howell-Jolly bodies are inclusion that may be seen in splenectomized patients or patients with an otherwise non-functioning or atrophic spleen, and in patients with severe anemia or leukemia.
Other common complications: Cerebral infarcts may occur from vaso-occlusion. Renal complications include nephrotic syndrome, glomerulosclerosis with proteinuria, papillary necrosis, and reduced concentrating capacity of the kidney. Priapism (painful, prolonged penile erection) may occur as recurrent episodes. Pulmonary hypertension may develop in long-standing cases.
Diagnosis and Treatment: Diagnosis is based on clinical features, peripheral smear showing sickle cells, a positive sickling test, and electrophoresis. Hb electrophoresis in SCA shows mainly HbS, absent HbA, and 2-20% HbF. Blood transfusions, desferrioxamine to treat iron overload, and bone marrow and stem cell transplant are used as therapy. Hydroxyurea (hydroxycarbamide) induces the production of HbF and is used in treatment.
Sign up for free to take 3 quiz questions on this topic