Anemia is a condition in which hemoglobin concentration and/or the RBC count is low, leading to decreased oxygen-carrying capacity of the blood. The World Health Organization (WHO) defines anemia as hemoglobin:
Classification of anemia: According to MCV, anemia can be classified as below.
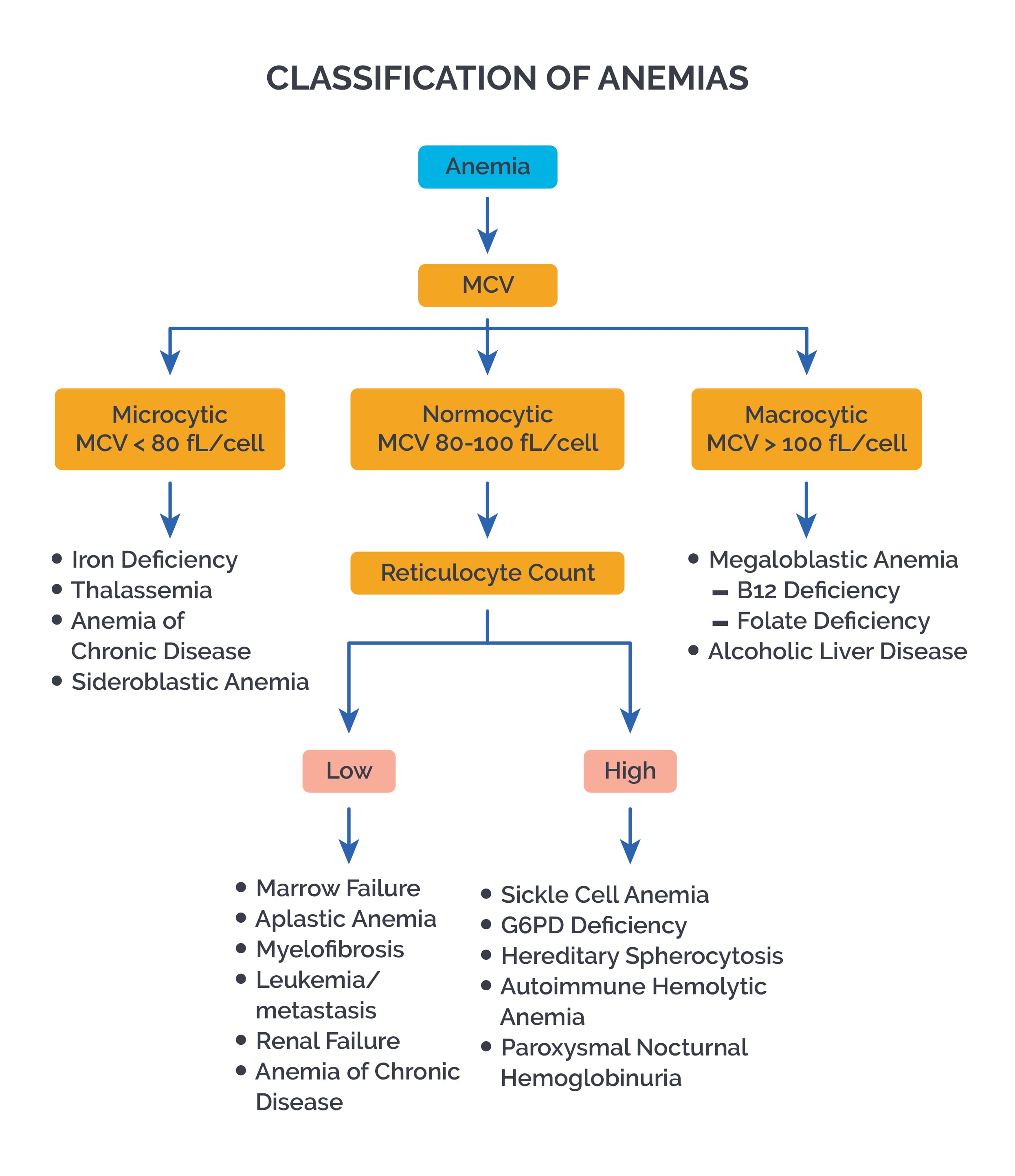
Microcytic: MCV<80 fL Seen in Iron deficiency anemia, Thalassemia, Sideroblastic anemia, Anemia of chronic disease, Lead toxicity, Copper deficiency
Macrocytic: MCV>100 fL Seen in Megaloblastic anemia (deficiency of Vit B12, folate; Pernicious anemia), Aplastic anemia, Myelodysplastic syndrome (MDS), Hypothyroidism, Liver dysfunction, Alcoholism, own Syndrome, Hb F, Drugs (methotrexate, phenytoin, mercaptopurine, Antiretroviral drugs), Fanconi anemia, Paroxysmal nocturnal hemoglobinuria (PNH)
Normocytic: MCV between 80-100 fL Seen in Acute blood loss, AOCD, Renal failure, Early stages of iron deficiency anemia, Hypothyroidism, Inflammation, Aplastic anemia, Hemolytic anemias
I) Microcytic Anemias
Microcytic anemia is defined as:
The most common causes are iron deficiency anemia (IDA) and thalassemia. Microcytosis results from deficient synthesis of heme and/or globin.
Iron deficiency anemia (IDA): IDA is most commonly caused by:
In IDA, iron stores (ferritin) become depleted first. This is followed by decreased hemoglobin and the development of hypochromic, microcytic anemia.
Clinical features include fatigue, hair loss, dyspnea on exertion, pallor, and pica. Patients with underlying CHD may develop angina due to reduced oxygen delivery.
On examination, you may see mucosal and scleral pallor, a smooth tongue, and koilonychia (spoon-shaped nails).
Iron studies show low serum iron, low ferritin, decreased Hb concentration, increased TIBC, decreased percent saturation of transferrin with iron, and increased free erythrocyte porphyrin. RDW is increased.
Peripheral smear shows hypochromic, microcytic RBCs, thrombocytosis, and anisocytosis, with a typically normal reticulocyte count and decreased RBC count. Bone marrow shows erythroid hyperplasia and increased RBC precursors. Serum transferrin receptor levels are elevated.
Plummer-Vinson or Paterson-Kelly syndrome presents as a classical triad of dysphagia, iron-deficiency anemia and esophageal webs. The syndrome is caused due to iron deficiency. It is typically seen in middle-aged females. The dysphagia is usually painless and intermittent or progressive over years, limited to solids and sometimes associated with weight loss. Glossitis, angular cheilitis and koilonychia are associated. It carries an increased risk of squamous cell carcinoma of the pharynx and the esophagus.
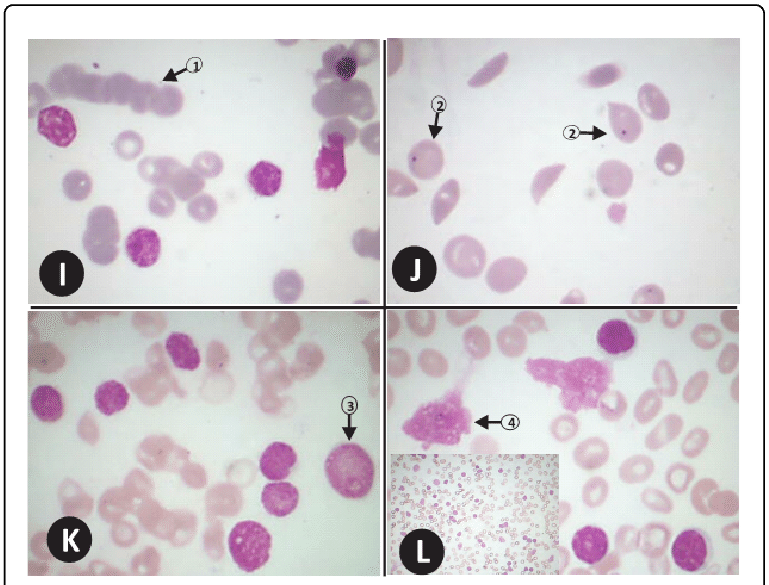
Anaemia morphology slides I-L. SLIDE I (Magnification x 1000): 1=rouleaux formation. SLIDE J (Magnification x 1000): 2=Howell jolly inclusion bodies in the cytoplasm of red cells of a 36 year old haemoglobin SS disease patient. SLIDE K (Magnification x 1000): 6=lymphoid blast (moderate size blast with scanty cytoplasm, high nuclear-cytoplasmic ratio, single prominent nucleolus). SLIDE L (Magnification x 1000, Inset x 400): 4=small (mature looking) lymphocyte; 5=Smear cells; Inset: Sea of mature looking, monomorphic lymphoid cells and smear cells seen in chronic lymphocytic leukaemia.
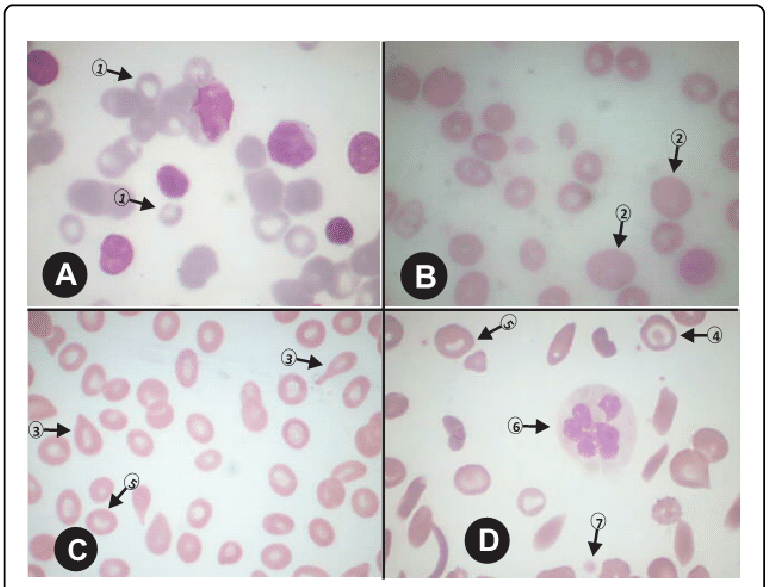
Anaemia morphology slides A-D. SLIDE A (Magnification x 1000): 1=microcyte. SLIDE B (Magnification x 1000): 2=oval macrocyte (compared to the nucleus of a mature lymphocyte). SLIDE C (Magnification x 1000): 3=tear drop red cell; 5=stomatocyte. SLIDE D (Magnification x 1000): 4=target red cell, 5=stomatocyte, 6=neutrophil hypersegmentation, 7=platelet/ thrombocyte.
Sign up for free to take 3 quiz questions on this topic