The liver occupies the right hypochondriac and epigastric regions. Normally, you can’t palpate it. In thin people, however, it may become just palpable under the right costal margin during deep inspiration.
The inferior border of the liver is curved and extends from the right 10th costal cartilage in the midaxillary line to the left 5th rib in the midclavicular line.
Liver span is the distance between the superior and inferior borders of the liver in the midclavicular line. It is typically 6-12 cm. Liver span increases in hepatomegaly.
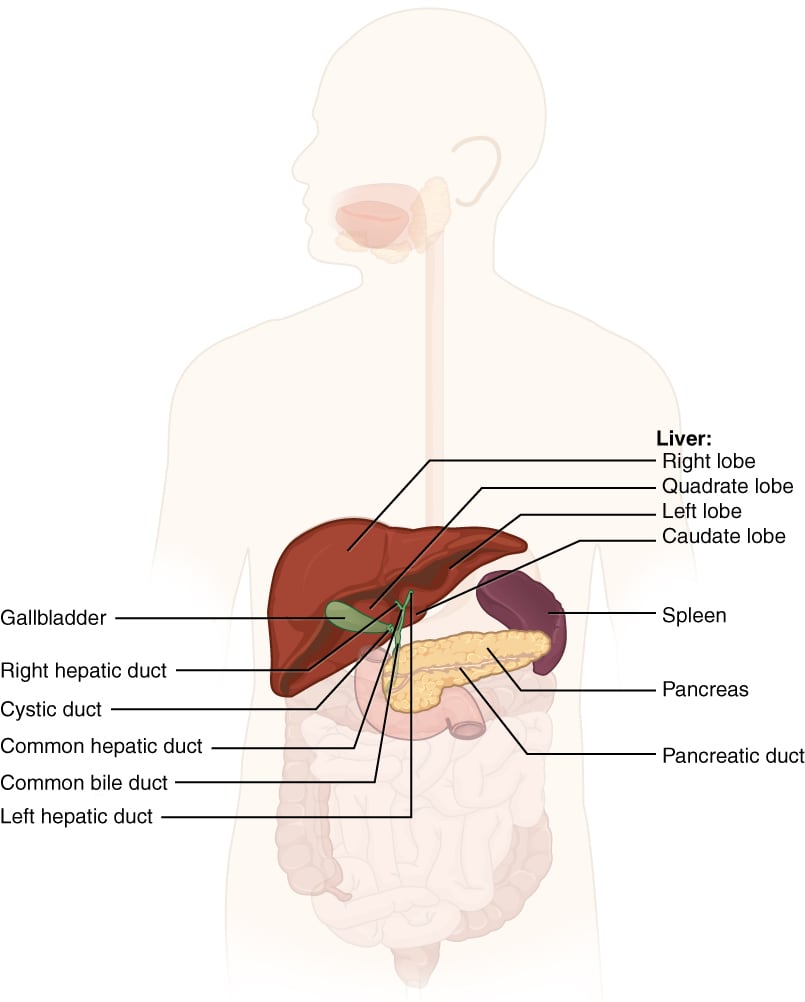
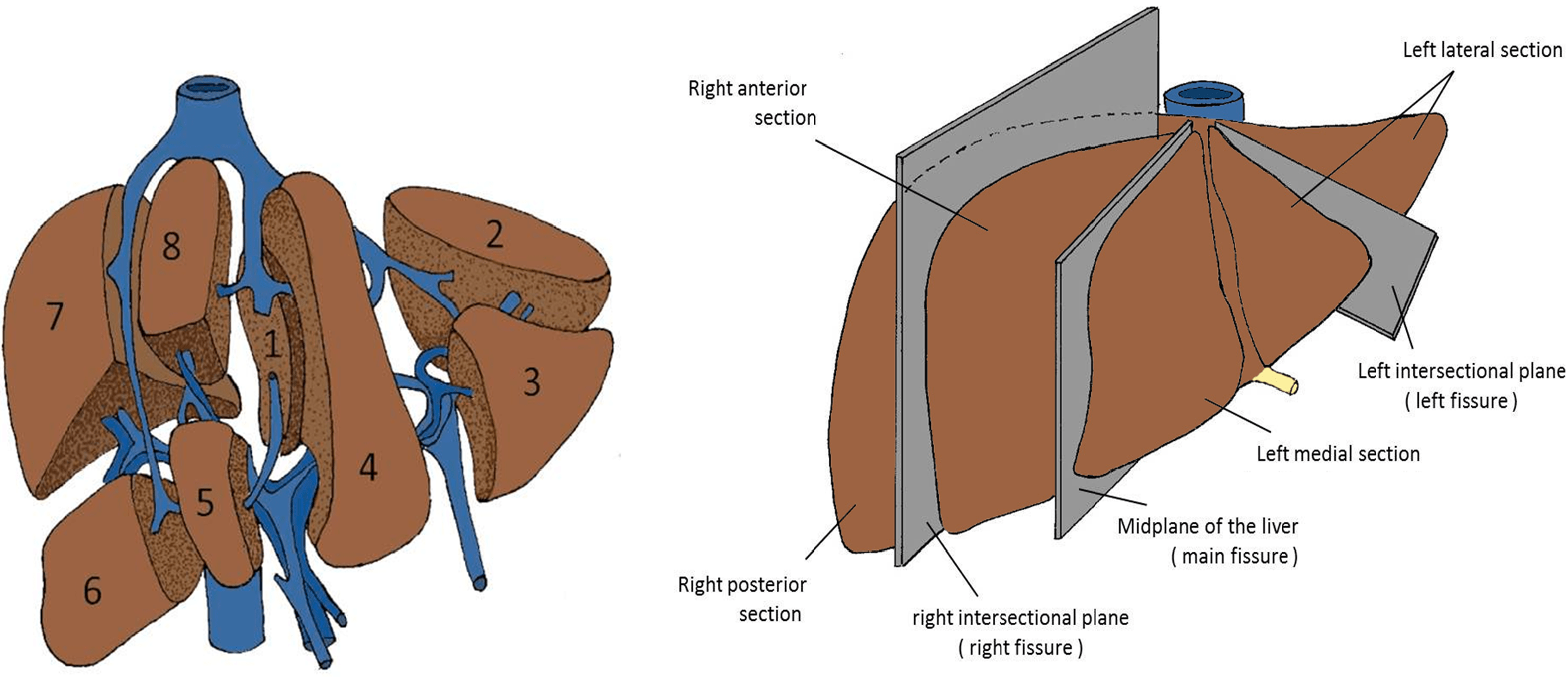
The liver is divided into a larger right lobe and a smaller left lobe. The caudate and quadrate lobes are part of the right lobe.
The connective tissue covering the liver is called Glisson’s capsule. It extends into the liver as sheaths surrounding the hepatic ducts, hepatic arteries, and portal tributaries. Glisson’s capsule continues into the hepatic ligaments.
The falciform ligament extends from the umbilicus to the anterior surface of the liver and continues as the coronary ligaments. The falciform ligament divides the liver anatomically (not functionally) into right and left lobes. Its lower edge contains the ligamentum teres (round ligament), a remnant of the left umbilical vein. The ligamentum venosum is present on the inferior surface.
In portal hypertension, the umbilical vein may recanalize, creating portosystemic collateral circulation and leading to caput medusae.
Other ligaments include the coronary and triangular ligaments. The ligaments of the liver help support it in the right upper quadrant of the abdomen. They are all avascular. The only exception is the IVC ligaments, which contain hepatic tissue.
The posterior surface of the liver is closely associated with the IVC (inferior vena cava), while the inferior surface is related to the gallbladder.
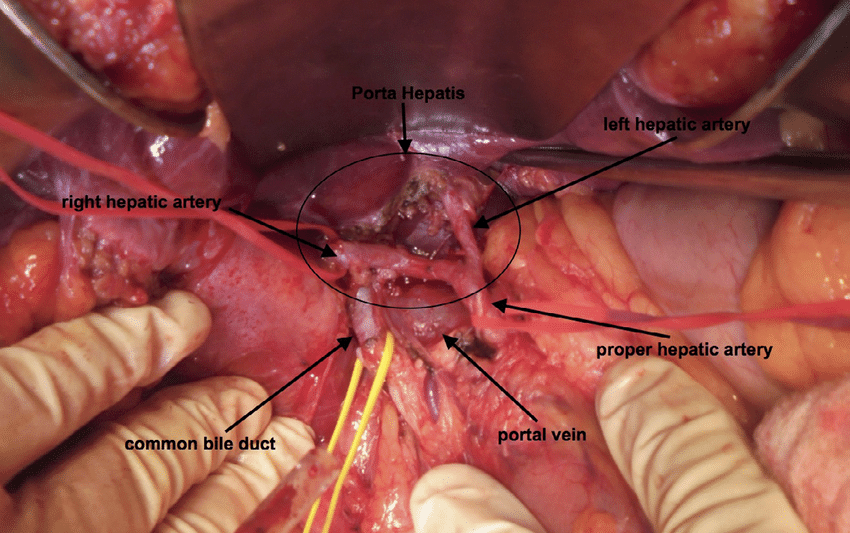
The porta hepatis (the “gateway” to the liver) lies on the inferior surface of the right lobe, between the caudate and quadrate lobes. From anterior to posterior, the structures at the porta hepatis are:
Nerve plexuses and lymphatics are also present at the porta hepatis.
The liver receives:
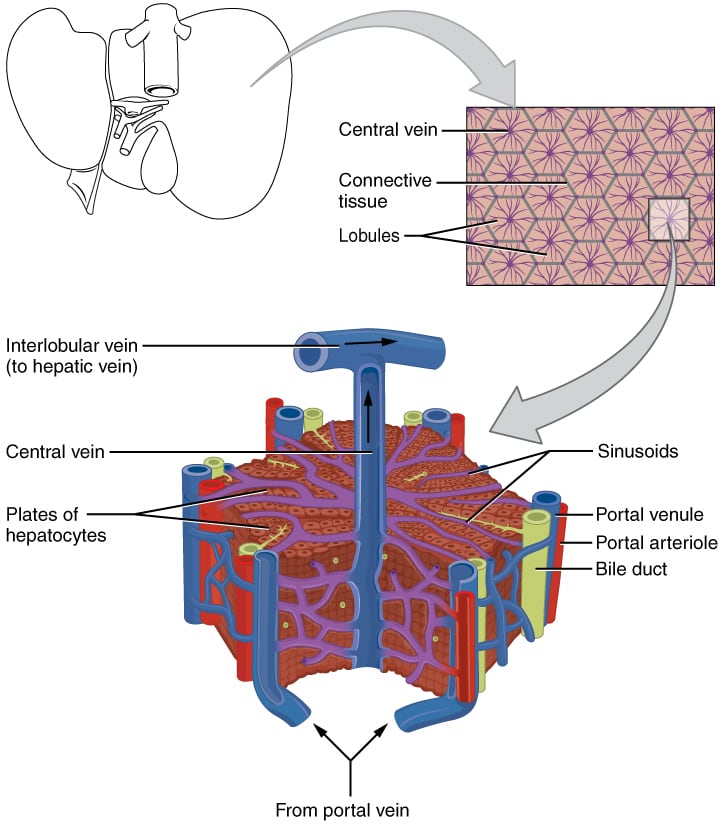
Blood from these two sources mixes in the hepatic sinusoids. The right and left hepatic arteries supply their respective lobes and give off interlobular branches that open into the sinusoids.
The portal vein carries:
It opens into the hepatic sinusoids. The hepatic sinusoids join to form the central vein, which ultimately unites to form the right, left, and middle hepatic veins that drain into the IVC.
The foramen of Winslow (epiploic foramen) is a communication between the greater sac and the lesser sac of the abdomen. It is located behind the hepatoduodenal ligament and below the caudate lobe of the liver.
The hepatoduodenal ligament contains the hepatic artery, portal vein, and common bile duct. The Pringle maneuver uses this anatomy to control hepatic bleeding by pinching off the major vessels supplying the liver (located in the hepatoduodenal ligament) by locating and applying pressure in the epiploic foramen.
Histologically, liver cells are arranged in hexagonal hepatic lobules, each with:
The portal triad consists of:
Blood flows from the periphery to the center, while bile flows from the center to the periphery.
The hepatic acinus is the functional unit of the liver. [It is not the same as the hepatic lobule ]. The acinus is an ellipsoidal area divided into three zones (1, 2, and 3), oriented along a line connecting two adjacent central veins.
| Zone | Associated pathology |
|---|---|
| 1 | Chronic hepatitis, primary biliary cirrhosis, obstruction of bile ducts, preeclampsia and eclampsia, phosphorus and ferrous sulphate poisonings, hemochromatosis |
| 2 | Yellow fever |
| 3 | Ischemic insults, acetaminophen toxicity, right heart failure, carbon tetrachloride poisoning, copper deposition, amanitin (mushroom) poisoning |
The hepatic macrophages are called Kupffer cells. They are found in the sinusoids.
Ito cells (also called stellate cells or lipocytes) are mesenchymal fat-storing cells located in the perisinusoidal space of Disse. They are involved in the storage and metabolism of vitamin A.
Following liver injury, Ito cells transform into activated myofibroblast-like cells. They secrete type I collagen and play a vital role in the development of cirrhosis. Collagen deposition by Ito cells in the space of Disse causes fibrosis and narrowing of the sinusoidal lumen, ultimately resulting in a buildup of pressure in the portal vein (portal hypertension). Ito cells also secrete cytokines and growth factors that promote regeneration of hepatic parenchymal cells.
It is formed at the level of the L2 vertebra by the joining of the superior mesenteric and splenic veins. It is located behind the neck of the pancreas. It divides into right and left branches at the porta hepatis.
This distribution is important in liver metastases from gastrointestinal viscera. In portal hypertension, blood is shunted from the portal veins to the systemic veins.
| Site of portosystemic anastomosis | Veins involved (portal system veins listed first) |
|---|---|
| Lower end of esophagus (esophageal varices) | Left gastric and esophageal/ hemiazygous veins |
| Around the umbilicus (caput medusae) | Paraumbilical veins and superior and inferior epigastric veins |
| Anal canal (internal hemorrhoids) | Superior rectal veins and inferior rectal veins |
| Bare area of liver | Hepatic portal veins with inferior phrenic veins |
The gallbladder is a pear-shaped organ located posteroinferior to the liver. It is anatomically divided into:
The fundus lies at the level of L1 at the transpyloric plane. The cystic duct drains the gallbladder.
Calot’s triangle is a space bounded by:
It contains the cystic artery and the lymph node of Lund. It is surgically important during cholecystectomy because the cystic artery and duct can be ligated in this triangle.
An outpouching may be seen at the junction of the neck and cystic duct called Hartmann’s pouch. It may dilate when obstructed by gallbladder stones.
The cystic duct joins the common hepatic duct to form the common bile duct.
The gall bladder mucosa is lined by columnar epithelium with microvilli. Rokitansky-Aschoff sinuses are a characteristic feature of the gallbladder and consist of deep mucosal outpouchings that extend beyond the musculais propria.
Sign up for free to take 6 quiz questions on this topic