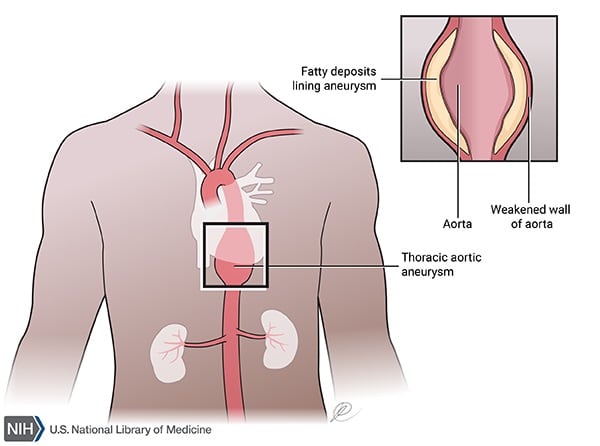
I) Aneurysms: An aneurysm is an abnormal dilation of a blood vessel. It’s seen most commonly in the abdominal aorta. Aneurysms are commonly described as saccular, fusiform, or cylindrical.
| Aneurysm type | Character |
| Atherosclerotic | Due to atherosclerotic damage to the vessel wall; more common after age 50 years; most common in the abdominal aorta (infrarenal location); risk of rupture increases with size (>5 cms); may present as a pulsatile abdominal mass |
| Cystic medial necrosis | Seen in old age, Marfan syndrome, and Ehler-Danlos syndrome; basophilic ground substance accumulates in the tunica media, which degenerates and develops cystic spaces; causes dissecting aneurysms (see below) |
| Syphilitic | Complication of syphilitic aortitis; involves the vasa vasorum, leading to ischemic damage of the aortic tunica media; located in the ascending aorta and arch of the aorta; “tree bark” appearance of the tunica intima; AR due to aortic root dilation |
| Mycotic aneurysms | Caused by infection of the arterial wall via direct spread or microembolization; more common in the aorta, peripheral arteries, and cerebral artery; most commonly caused by Staphylococcus, Streptococcus, and Salmonella; higher risk in IV drug users and in infectious endocarditis, DM, and malignancies; risk of rupture and fulminant sepsis |
| Berry aneurysms | Small, berry-like aneurysms that form in the circle of Willis |
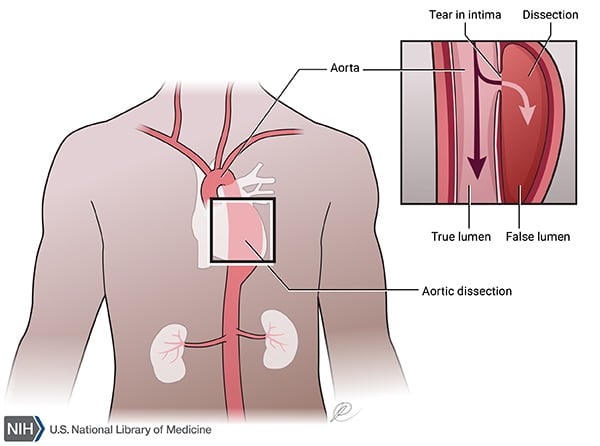
Dissecting aneurysms: This refers to vessel dilation associated with formation of a vessel wall hematoma, typically after a tear in the tunica intima. There is no true aneurysm formation.
Common causes include older age, hypertension, pregnancy, coarctation of the aorta, trauma, and any condition causing cystic medial necrosis (e.g., Marfan syndrome). It’s most common in the ascending aorta.
The hematoma collects in the tunica media and may extend into aortic branches and the abdominal aorta. Dissections are classified as:
Type A is managed surgically, while type B can be medically managed.
Patients may present with excruciating, tearing pain in the anterior or posterior chest, AR if the aortic valve is involved, STEMI from coronary artery involvement (don’t give anticoagulants in AMI from dissection), cardiac tamponade, shock, weakened pulses, and organ ischemia (e.g., abdominal ischemia, stroke). Complications include retroperitoneal hemorrhage, collapse, and death. X-ray may show a widened mediastinum and a double aortic contour.
II) Peripheral arterial disease or arteriosclerosis obliterans: Peripheral vascular (arterial) disease is systemic atherosclerosis affecting arteries distal to the arch of the aorta. In some cases, it may occur due to embolisation.
Risk factors include age older than 60 years, smoking, hypertension, DM, hyperhomocysteinemia, elevated CRP, elevated lipoprotein A, insulin resistance, chronic renal insufficiency, and dyslipidemia.
It typically presents with leg pain during activity (intermittent claudication), such as walking, that improves with rest. Pain may occur in the buttocks, hips, thigh, or calf. The pain location helps localize the disease:
On examination, you may see muscle atrophy, loss of hair with smooth, shiny skin over the affected area, decreased or absent pulses in the feet, non-healing leg ulcers, and cold or numb toes. Ulcers have a punched-out appearance, with a gray or yellow fibrotic base and undermined edges.
Erectile dysfunction may occur either alone or as part of Leriche syndrome, caused by atherosclerotic stenosis of the abdominal aorta at its bifurcation into the iliac arteries. In advanced disease, livedo reticularis may be seen. There is an increased risk of CAD.
ABI (ankle-brachial index) is calculated as the ratio of systolic pressure in the ankle to brachial pressure, measured in the supine position. A normal ratio is greater than 1. An ABI less than 0.9 is consistent with PVD; in severe disease, ABI is < 0.5. Pressure is measured by doppler ultrasound at the brachial artery and posterior tibial artery. Arteriography is the gold standard for diagnosis.
III) Arteriovenous fistula: An arteriovenous (AV) fistula is an abnormal connection between an artery and a vein without intervening capillaries. It may be congenital or acquired.
Congenital fistulas may be seen in Osler-Weber-Rendu syndrome (hereditary hemorrhagic telangiectasias). Acquired causes include penetrating trauma, cardiac catheterization, or medical creation for dialysis.
AV fistulas may appear as purplish, bulging vessels with local swelling. Larger AV fistulas can cause symptoms due to shunting, including hypotension, high-output heart failure, fatigue, and diversion of blood flow leading to ischemic symptoms in the local area supplied. They predispose to thromboembolism and internal bleeding. A machinery murmur may be heard over the fistula.
Sign up for free to take 4 quiz questions on this topic