I) Premature atrial complexes (PACs): PACs are premature beats that arise from an ectopic pacemaker in the atria. On ECG, you’ll see an abnormal P wave followed by a normal QRS complex. A post-extrasystolic pause is often present, meaning there’s a longer-than-normal interval before the next sinus beat. PACs may be unifocal or multifocal.
They can occur in repeating patterns such as:
Patients may describe “skipped beats.” PACs may be benign or associated with IHD, left atrial enlargement, WPW syndrome, anxiety, beta agonists, caffeine, digoxin toxicity, IHD, sympathomimetics, etc.
II) Atrial tachycardia (AT): Atrial tachycardia is a type of supraventricular tachycardia in which the atria beat at rates higher than 100/min. The impulse originates from an ectopic site in the atria (not the SA node). Patients may present with palpitations, chest discomfort, dyspnea, dizziness, and rarely syncope.
Because the rhythm is not sinus, the P-wave morphology will be slightly different from the normal sinus P wave. Atrial tachycardia is seen in children with CHD, the elderly, hypertension, cardiomyopathy, and alcohol or cocaine abuse, etc.
Atrial tachycardia may be focal or multifocal:
Multifocal AT is commonly seen in lung disorders such as PE and COPD, etc.
III) Atrial flutter: Atrial flutter is a rapid but regular rhythm with atrial rates between 250-350 beats/minute. It occurs due to re-entry circuits within the atria. ECG shows regular, sawtooth-like flutter waves.
IV) Atrial fibrillation: Atrial fibrillation is characterized by disorganized electrical activity in the atria. Symptoms may include syncope, collapse, and palpitations, etc. It is seen in old age, HT, IHD, CCF, RHD, hyperthyroidism, alcohol abuse, and electrolyte abnormalities.
ECG shows an irregular rhythm with absent P waves and a changing R-R interval. The ECG baseline shows fibrillatory waves with frequencies as high as 600/minute.
V) Atrioventricular (AV) nodal re-entrant tachycardia (AVNRT): AVNRT is the most common type of SVT. It may present with palpitations, dizziness, dyspnea, or syncope. AVNRT is caused by a re-entrant circuit near the AV node.
It involves a fast and a slow pathway. Most commonly, the slow pathway is used for anterograde conduction from atria to ventricles, while the fast pathway is used for retrograde conduction. This is called slow-fast AVNRT. Premature atrial or ventricular contractions may precipitate AVNRT. Caffeine, tobacco, alcohol, stress, or exercise may trigger AVNRT.
ECG shows a narrow-complex tachycardia at rates typically between 120-240 beats per minute, and P waves cannot be discerned.
Valsalva maneuver, intravenous adenosine, and carotid sinus massage may terminate SVTs by vagal activation. Cerebral stroke from carotid thrombus embolization can occur as a result of carotid sinus massage.
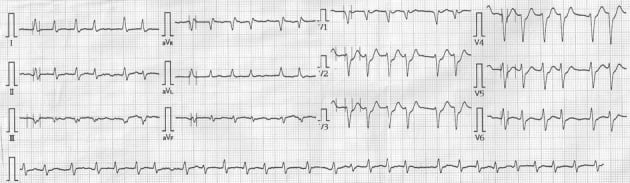
VI) WPW syndrome (Wolff-Parkinson-White syndrome; pre-excitation syndrome): The underlying pathology is early depolarization of the ventricular myocardium before normal conduction through the AV node has occurred. Early and faster conduction occurs through an accessory pathway called the Bundle of Kent, which connects the atria to the ventricle.
On ECG, WPW is characterized by a “delta wave” at the onset of the QRS complex. Drugs that block conduction through the normal AV junction (such as adenosine, calcium channel blockers, and digoxin) are contraindicated in WPW syndrome because they enhance conduction through the Bundle of Kent and can precipitate ventricular tachycardia.
VII) Ventricular ectopic beats (VPCs; ventricular premature complexes): These are premature beats that result from abnormal excitation of the ventricles. They are typically benign. They may be associated with CAD, stimulants such as caffeine and pseudoephedrine, AMI, etc.

VIII) Ventricular tachycardia: Ventricular tachycardia is a broad-complex ventricular arrhythmia with a rate > 100/min. It can be diagnosed when more than three consecutive ventricular premature complexes occur in a row.
Depending on duration, VT may be:
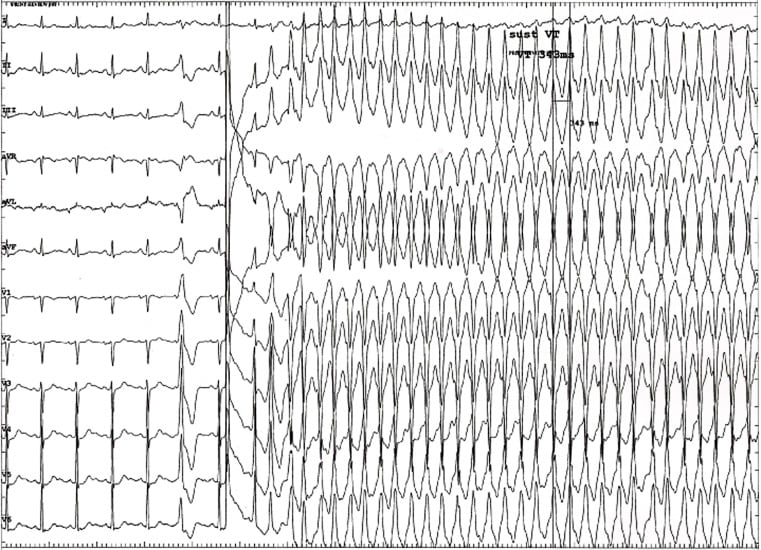
IX) Torsades de pointes: Also called polymorphic ventricular tachycardia. ECG shows the characteristic “turning of points” along the baseline due to a changing axis. It is seen in electrolyte disturbances such as hypomagnesemia and hypokalemia, and in factors that prolong the QT interval such as congenital long QT syndrome, antiarrhythmics, TCAs, Romano-Ward syndrome, etc. It may precipitate ventricular fibrillation (VF).
X) Ventricular fibrillation: Ventricular fibrillation is a chaotic, irregular ventricular rhythm and is potentially fatal. The ventricles fail as a pump because contraction is not coordinated. It is seen in AMI, CAD, cardiomyopathies, heart failure, long QT syndrome, Brugada syndrome, drugs, etc.
ECG shows chaotic waves without any regularity or rhythm and without identifiable P waves or QRS-T complexes. The rate is typically very high, ranging from 150-500/minute.
XI) Atrioventricular block (AV block): In AV block, conduction of electrical impulses from the atria to the ventricles is delayed or blocked. AV block may be first degree, second degree, or third degree.
In first degree AV block, the PR interval is prolonged more than 200 milliseconds (>1 big ECG square). It is seen in myocarditis, IHD, degenerative diseases of the conduction system, or drugs such as TCAs. No treatment is needed for first degree block.
Second degree block can be type I or type II:
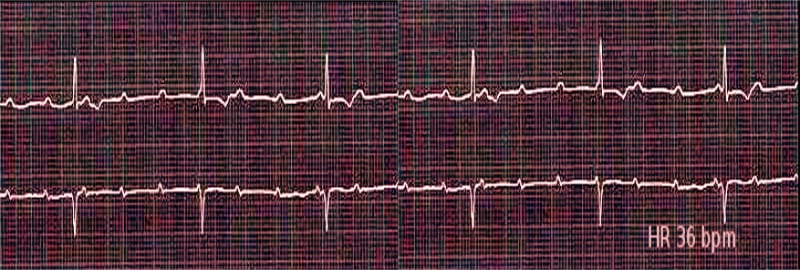
Third degree heart block is also called complete heart block. There is complete dissociation of P waves from the QRS complexes. The atria beat at their own rate while the ventricles beat at a slow intrinsic rate of 30-40 beats/min. It is seen in IHD and drug toxicity with beta blockers, digitalis, and calcium channel blockers. A permanent pacemaker is essential.
XII) LBBB and RBBB: Bundle branch blocks occur due to conduction blocks in either the right or left bundle branches.
Sign up for free to take 3 quiz questions on this topic