IHD results from an imbalance between myocardial oxygen demand and oxygen supply. The most common cause of IHD is atherosclerotic disease of the coronary arteries, also called CAD (coronary artery disease). CAD most commonly involves the left anterior descending (LAD) branch of the left coronary artery, followed by the right coronary artery (RCA) and the left circumflex artery (LCx). Significant coronary stenosis occurs when there is more than a 75% decrease in the vessel lumen.
Risk factors include male gender (> 45 years of age), post-menopausal females, smoking, DM, insulin resistance, older age, family history of premature CAD, hypertension, hypercholesterolemia, and dyslipidemia.
I) Angina pectoris: Angina pectoris is chest pain caused by transient myocardial ischemia that is not severe enough to cause cell death. Patients with typical (stable) angina usually describe poorly localized pain or discomfort in the retrosternal area and/or arm that is exacerbated by exertion or emotional stress and relieved by rest and nitroglycerine. Tenderness to palpation is not a characteristic of anginal pain.
Angina is of the following three types:
II) Acute coronary syndrome or ACS: ACS refers to symptoms caused by acute myocardial ischemia and includes ST elevation MI (STEMI), non-ST elevation MI (NSTEMI), and unstable angina. It may present as sudden cardiac death, so prompt management is essential.
The most common mechanism of AMI (acute myocardial infarction) is hemorrhage or ulceration of an atherosclerotic plaque, leading to thrombosis that closes off an already narrowed lumen. In AMI, the affected myocardium undergoes irreversible necrosis. Non-atherosclerotic causes can rarely cause AMI, such as vasculitis, coronary arterial stenosis, severe coronary spasm, aortic dissection, hypercoagulability, etc.
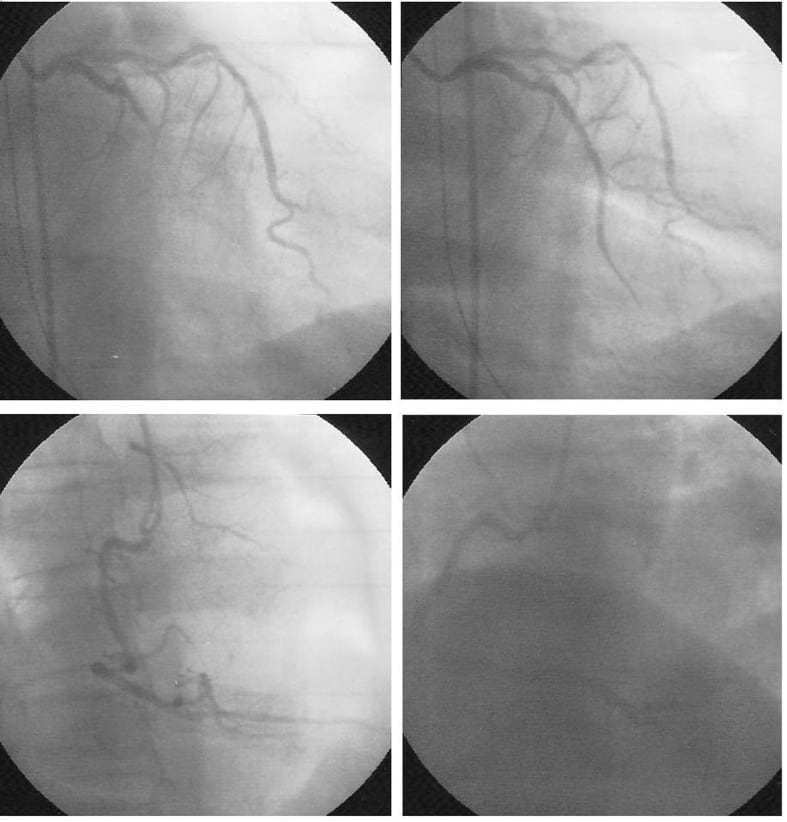
(Upper panel) coronary angiography of left coronary artery shows total occlusion on the mid portion of left circumflex artery (left), and after stent deployed (right); (lower panel) coronary angiography of right coronary artery.
Patients typically present with retrosternal chest pain often described as crushing or pressure, with radiation to the neck, jaw, left shoulder, or left arm. Associated symptoms can include diaphoresis, fatigue, epigastric pain, nausea, vomiting, or syncope. The pain typically lasts more than 30 minutes and is not relieved by rest or nitroglycerine. Variations of the classic presentation are seen in diabetics and women.
AMI may be full-thickness (transmural), or it may be subendocardial, where only the inner third of the myocardium is infarcted (this area is perfused last). Coronary thrombosis may or may not be present in subendocardial infarcts; the main pathology is hypoperfusion, as in shock and aortic stenosis.
| Time since AMI | Gross changes | Microscopic changes |
| 0-6 hours | No change | Hypereosinophilic myocardium, wavy fibres, EM changes# |
| 6-12 hours | Infarcted area appears whitish or pale while non-infarcted area appears brick-red on TTC stain* | Coagulative necrosis starts; Early neutrophilic infiltrates; edema |
| 12-24 hours | Dark mottling | Progression of above changes; more prominent neutrophilic infiltrates |
| Days 1-3 | Pallor; mottled area with a yellow tan core | Loss of nuclei and striations on myocytes; abundant neutrophils |
| Days 3-7** | Yellow and soft centre; hyperemic border | Myocyte fragmentation; early phagocytosis; macrophages appear; early granulation tissue |
| Days 7-10 | Bright yellow necrotic area; red-purple periphery | Prominent granulation tissue; necrosis is complete (in smaller infarcts); loose collagen; pigmented macrophages*** containing hemosiderin and lipofuscin |
| Days 10-14 | Red-grey borders | Fibrocollagenous tissue at periphery |
| Weeks 2-8 | Thin, grey-white, fibrous scar | Denser collagen, scanty cells |
| Month 2-3 | Scarring complete | Mature collagen |
| Changes in reperfusion injury | Hemorrhagic, red infarct area | Contraction band necrosis |
*TTC (triphenyltetrazolium chloride) is a histochemical stain used to differentiate between infarcted and non-infarcted tissue. It depends on the activity of dehydrogenases in metabolically active cells.
**Because the infarcted area is soft, the risk of cardiac rupture is maximal from days 3-7.
***Pigmented macrophages may persist for years.
#EM (electron microscopy) changes can be seen within a few minutes of the infarct. Swollen mitochondria, disruption of sarcolemma, clumping of nuclear chromatin, and glycogen depletion occur within the first 30 minutes of infarction.
Sign up for free to take 6 quiz questions on this topic