Cholelithiasis or gallstones: This is the presence of solid calculi in the gallbladder. Calculi form when bile becomes supersaturated and precipitates. Gallstones may be:
Risk factors include high-calorie diet, obesity, female sex, pregnancy, rapid weight loss, estrogen therapy, cholestasis, low physical activity, diabetes mellitus, dyslipidemias, total parenteral nutrition, low fibre diets, hyperinsulinism, and metabolic syndrome.
Many people are asymptomatic. Others present with biliary colic, which is acute abdominal pain in the RUQ or epigastrium. It may be aggravated by fatty foods and typically resolves gradually over 1-5 hours. Upper abdominal tenderness is present. Some patients progress to complications (e.g., acute cholecystitis).
Gallstones can be visualized on ultrasound.
Management
Complications of gallstones: As follows
Acute cholecystitis: This is acute inflammation of the gallbladder caused by obstruction of the cystic duct by a gallstone. There is often a past history of recurrent biliary colic. It presents with RUQ pain, fever, and chills. An RUQ mass may be palpable. A positive Murphy sign is present (inspiratory arrest on deep palpation in the RUQ).
Laboratory findings include leukocytosis and slightly elevated bilirubin.
Diagnosis
Treatment
Gangrenous cholecystitis: This is necrosis and perforation of the gallbladder wall due to ischemia from progressive vascular insufficiency, occurring as a complication of gallstones. It is seen in diabetics, older age, delayed surgery for acute cholecystitis, and cardiovascular disease. It carries a very high mortality rate.
Imaging
Treatment is laparoscopic or open cholecystectomy plus supportive management including antibiotics.
Emphysematous cholecystitis: This is seen with infections due to Clostridia, E.coli, and other gas-forming organisms. It is rapidly progressive and can lead to gangrene. It is more common in older patients and diabetics.
Treatment is antibiotics plus open cholecystectomy or percutaneous cholecystostomy (in some cases).
Acalculous cholecystitis: This is inflammation of the gallbladder caused by hypo- or dyskinesia of the gallbladder with reduced emptying, in the absence of stones. It can follow long periods of fasting or starvation, TPN, rapid weight loss, critical illness (ICU patients), severe burns, and surgery. It has a high mortality rate because gangrene and perforation are common.
Patients present with typical symptoms of acute cholecystitis plus sepsis and shock.
Diagnosis
Management
Choledocholithiasis and ascending cholangitis: Gallstones may migrate into the common bile duct.
Cholangitis presents with Charcot’s triad:
If severe with septicaemia, Reynolds pentad develops:
This is a medical emergency and should be treated with intravenous antibiotics and ERCP to retrieve the stone. ERCP is both diagnostic and therapeutic.
Treatment is antibiotics and ERCP with or without stenting.
Gallstone pancreatitis: A stone may migrate further and block the opening of the pancreatic duct at the level of the Sphincter of Oddi, causing pancreatitis.
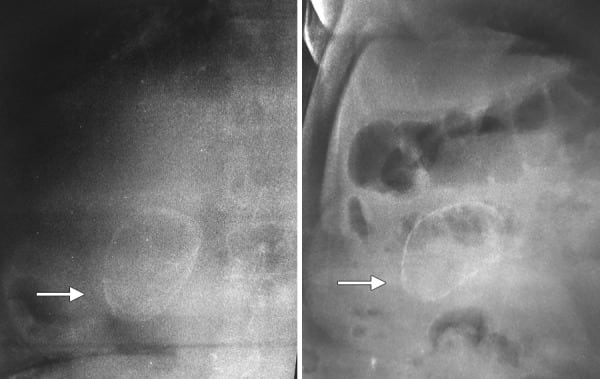
Gallstone ileus: This is mechanical obstruction of the intestine caused by an impacted gallstone. It typically follows acute cholecystitis. Inflammation leads to pressure and ischemic necrosis of the gallbladder wall, adhesions, and formation of a cholecysto-enteric fistula. The gallstone enters the intestine through the fistula and obstructs the intestine, most commonly the terminal ileum.
Patients present with nausea, vomiting, crampy abdominal pain, and abdominal distension. Jaundice may be present. Perforation peritonitis may occur.
Imaging studies show:
Treatment is supportive, with stone removal and closure of the fistula. Some cases may require bowel resection.
Sign up for free to take 4 quiz questions on this topic