The brain is vulnerable to trauma because soft brain tissue sits inside a hard skull with relatively little extra space. CNS trauma is commonly seen in motor vehicle accidents, sports injuries, falls, and acts of violence. The following types are seen:
(I) Parenchymal brain damage: Trauma to the brain can cause a concussion, which is characterized by transient neurological dysfunction and loss of consciousness without any morphologic changes. Diffuse axonal injury may be present.
Repeated concussions (for example, in sports) can lead to dementia, irritability, insomnia, and emotional disturbances, called post-concussion syndrome.
Dementia pugilistica (chronic traumatic encephalopathy), also called “punch-drunk syndrome” or “boxer’s dementia,” is a form of dementia that poses a serious long-term threat to individuals involved in contact-heavy sports (such as boxing) or to those who have sustained multiple concussions over their lifetime. Symptoms typically appear about 10-15 years after the injuries. Clinical features mimic Alzheimer’s syndrome.
Blunt brain trauma can also cause contusions, which involve damage to small blood vessels.
Both diffuse axonal injury and contusions can occur after sudden acceleration-deceleration injuries.
Diffuse axonal injury is classically seen with sudden angular acceleration or deceleration. Axonal shearing occurs as the cerebrum moves back and forth over a relatively fixed brainstem.
(II) Epidural haematoma: Blood collects between the dura and the skull. It typically follows fractures of the temporal or parietal bones that rupture the middle meningeal artery. The haematoma does not usually cross suture lines.
An asymptomatic or lucid interval may occur after trauma, followed later by neurological deterioration. Imaging shows a hyperdense, biconvex (lentiform) mass. More translucent areas may be seen with active bleeding or older hematomas.
(III) Subdural haematoma: Blood collects under the dura mater, between the dura and arachnoid mater. It results from rupture of bridging veins between the dural venous sinuses and the brain. It can be acute or chronic.
Chronic subdural hematoma is associated with brain atrophy, which predisposes bridging veins to rupture. It may cause dementia.
On noncontrast CT scan:
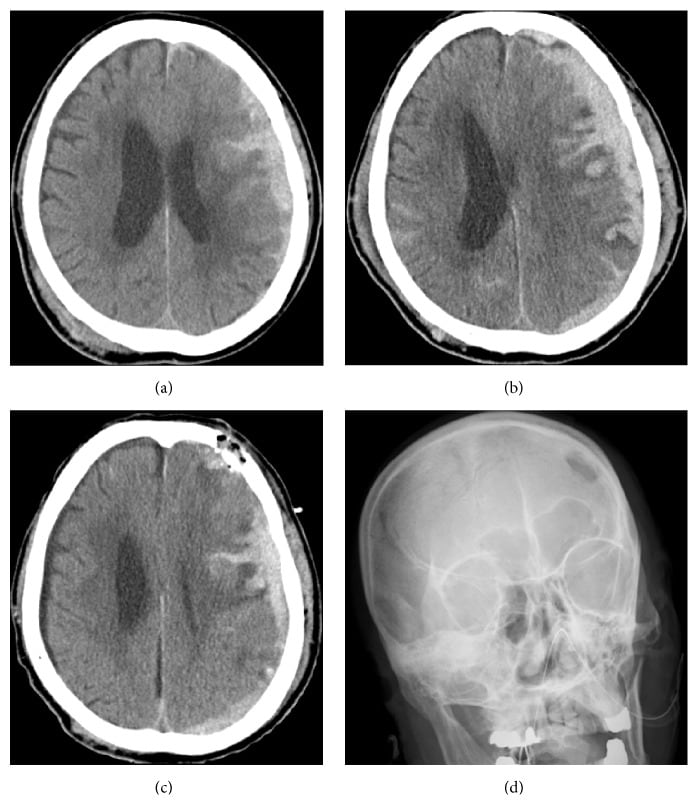
a) Axial plain CT scan at the time of admission shows left acute subdural hematoma and bilateral frontal contusion with thickness of 14 mm and midline shift of 8 mm. There is a bruised area in the right parietal region without bone fracture. (b) Axial plain CT scan 72 hours after admission shows worsened acute subdural hematoma with thickness of 16 mm and midline shift of 9 mm. Massive contusion of the left frontal lobe has occurred. © Axial plain CT scan after surgery shows reduced hematoma. Midline shift had improved to 4 mm. There is a small amount of air in the subdural space. Burr hole is covered by bone powders. (d) Radiographic frontal view shows the location of the burr hole 4 cm above the left eyebrow.
(IV) Shaken baby syndrome: This occurs due to child abuse involving vigorous shaking of an infant. It causes traumatic brain injury and sometimes cervical spine injury, and it may be associated with HIE.
Infants may present with coma, hypotonia, apnea, lethargy, vomiting, etc. Characteristically, subdural hematoma and retinal hemorrhages are seen.
Sign up for free to take 6 quiz questions on this topic