Spinal cord disorders
(I) Vertebral artery dissection: Vertebral artery dissection is characterized by a tear in the vascular wall. Blood enters the wall layers and forms an intramural haematoma, which narrows the vessel lumen and can cause ischemia. It is a common cause of stroke in younger age groups, including children. Many patients have weak arterial walls due to Ehlers-Danlos syndrome, Marfan’s syndrome, ADPKD, and osteogenesis imperfecta type I. Mechanical stress on the neck (for example, certain types of yoga, painting a ceiling, or chiropractic manipulation of the neck) has been associated with vertebral artery dissection. Some cases have a history of respiratory viral infection.
It can be:
- Ischemic type, manifesting with symptoms of vertebrobasilar system infarction
- Hemorrhagic type, presenting as subarachnoid hemorrhage
The vertebral artery is most mobile (and therefore most vulnerable to mechanical injury) at C1 to C2, as it leaves the transverse foramen of the axis vertebra and suddenly turns to enter the intracranial cavity. It presents with severe neck pain followed by dizziness, vertigo, double vision, ataxia, and dysarthria, often with lateral medullary syndrome and cerebellar infarction.
Angiography shows:
- “String sign”: a long segment of narrowed lumen
- Intimal flap or a double lumen
- Aneurysmal dilatations
- Sudden tapering due to occlusion of the lumen
(II) Spinal artery thrombosis/embolism: In adults, this is caused by atherosclerotic disease, thoracoabdominal aneurysms, aortic surgery, hypotension, diving, sickle cell anemia, coagulopathies, and spinal arteriovenous malformations. In children, cardiac defects and trauma are the leading causes. Clinically, it can present as anterior or posterior spinal artery syndrome.
Anterior spinal artery syndrome
- Involves anterolateral parts of the spinal cord
- Bilateral loss of motor function, pain and temperature sensations due to involvement of corticospinal and spinothalamic tracts
- Spinal shock initially, followed by spasticity and hyperreflexia
- Autonomic dysfunction, sexual dysfunction, bowel-bladder dysfunction
- Respiratory failure if cervical cord involved
- Dorsal columns are spared
Posterior spinal artery syndrome
- Involves dorsal columns
- Loss of proprioception and vibration below the level of lesion
- Anaesthesia at the level of lesion
- Can be unilateral or bilateral
(III) Spinal cord compression: Spinal cord compression can occur due to trauma, vertebral compression fractures, disk herniation, infection, and primary or metastatic tumors. Lung, breast, prostate, and renal cancer metastases commonly cause cord compression. Acute cord compression is a medical emergency.
Cord compression presents with paresis, sensory changes or loss of sensation, bowel-bladder sphincter dysfunction, and erectile problems. Treatment includes administration of corticosteroids, radiation therapy, surgery, and chemotherapy.
(IV) Hemisection of the spinal cord or Brown-Sequard syndrome: This is usually caused by trauma, tumors, or a herniated disc.
Clinical features of Brown-Sequard syndrome
- Ipsilateral spastic paralysis below the level of lesion
- Ipsilateral loss of tactile discrimination, vibration, joint position and pressure sensations below the level of lesion
- Contralateral loss of pain and temperature sensations 1 or 2 segments below the lesion
- If lesion at cervical cord then ipsilateral Horner;s syndrome
- Ipsilateral loss of all sensations and ipsilateral flaccid paralysis at the level of lesion
Soon after complete transection or hemisection of the spinal cord, there is a variable period of spinal shock characterized by loss of all reflexes, flaccid paralysis, and loss of all sensations below the level of the lesion.
(V) Spinal stenosis (cervical, lumbar): Spinal stenosis is narrowing of the spinal canal. It usually results from acquired degenerative changes (spondylosis), although congenital stenosis is sometimes seen. Other causes include osteoarthritis, tumors, rheumatoid arthritis, trauma, achondroplasia, and Paget’s disease.
Spinal stenosis can involve the cervical, thoracic (rarely), or lumbar spine.
- Cervical or thoracic spinal stenosis can cause root and/or cord compression, resulting in pain, radiculopathy, myelopathy, or myeloradiculopathy.
- Lumbar spinal stenosis causes only root compression, with typical complaints of neurogenic claudication or radicular leg pain.
Neurogenic claudication consists of pain in the buttocks or legs, typically aggravated by walking, standing, climbing stairs, or walking uphill, and alleviated by sitting or bending forward (lumbar flexion). Patients with spinal stenosis may also experience numbness, weakness, and loss of reflexes.
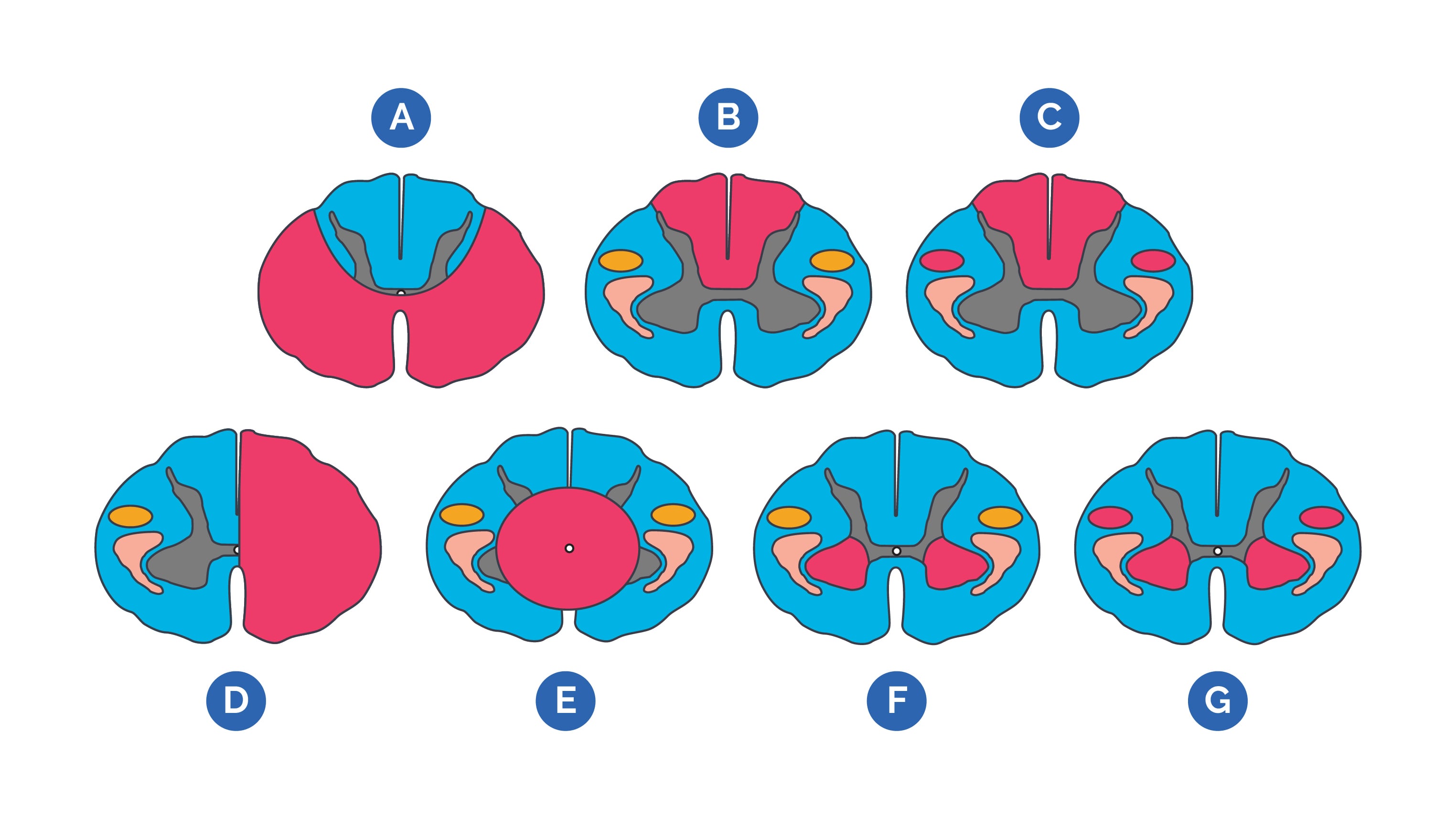
A. Anterior cord syndrome/infarct
B. Posterior cord syndrome or tabes dorsalis of tertiary syphilis
C. Subacute combined degeneration from B12 deficiency
D. Brown-Sequard cord hemisection
E. Central cord syndrome or syrinx (syringomyelia)
F. Poliomyelitis
G. Amyotrophic lateral sclerosis
(VI) Other important lesions involving the spinal cord
| Lesion | Characteristics |
| Syringomyelia | Cavitation of the central canal of the spinal cord, most common in the cervical canal; bilateral loss of pain and temperature (cape like distribution) at or just below the level due to compression of crossing spinothalamic fibres in the ventral commissure; CSF filled cavity called a syrinx; as the syrinx expands, increased compression causes LMN and ventral horn symptoms such as flaccid paralysis of upper limbs; Horner’s syndrome. |
| ALS (amyotrophic lateral sclerosis) or Lou-Gehrig’s syndrome | Affects both UMNs and LMNs; either upper or lower limb involvement; cranial nerve nuclei may be involved; cervical lesions present with flaccid weakness of upper limbs and spastic weakness of lower limbs; difficulty swallowing and speaking; respiratory failure in phrenic nerve involvement |
| Werdnig-Hoffmann disease or infantile spinal muscular atrophy | Destruction of LMNs in infants and young children; difficulty sucking, swallowing, breathing; limb weakness; “floppy babies”; symmetric involvement |
| Poliomyelitis | Flaccid paralysis, hyporeflexia, fasciculations, muscle atrophy, loss of LMNs in ventral horn, asymmetric involvement |
| Tabes dorsalis (neurosyphilis) | Bilateral degeneration of large diameter dorsal root fibres and their cell bodies in dorsal root ganglion; degeneration of dorsal columns esp. Fasciculus gracilis; pain, paresthesias and polyuria |
| Subacute combined degeneration | Degeneration of dorsal columns and corticospinal tracts; bilateral spastic paresis, bilateral numbness, gait disturbances, loss of touch, pressure, vibration senses below the level of lesion; peripheral neuropathy with paresthesias; Causes are Vit B12, Vit E (also involves spinocerebellar tract), copper and folic acid deficiency. |