(I) Adrenoleukodystrophy: This is an X-linked disorder characterized by accumulation of very long-chain fatty acids (VLCFAs) in peroxisomes due to a defect in beta-oxidation of VLCFAs. The buildup of VLCFAs leads to immune-mediated destruction of myelin, causing cerebral demyelination and peripheral neuropathy, along with adrenocortical and testicular insufficiency.
Clinical manifestations include seizures, spastic tetraplegia, dementia, hyperactivity, and features of Addison’s disease. Most cases present in childhood.
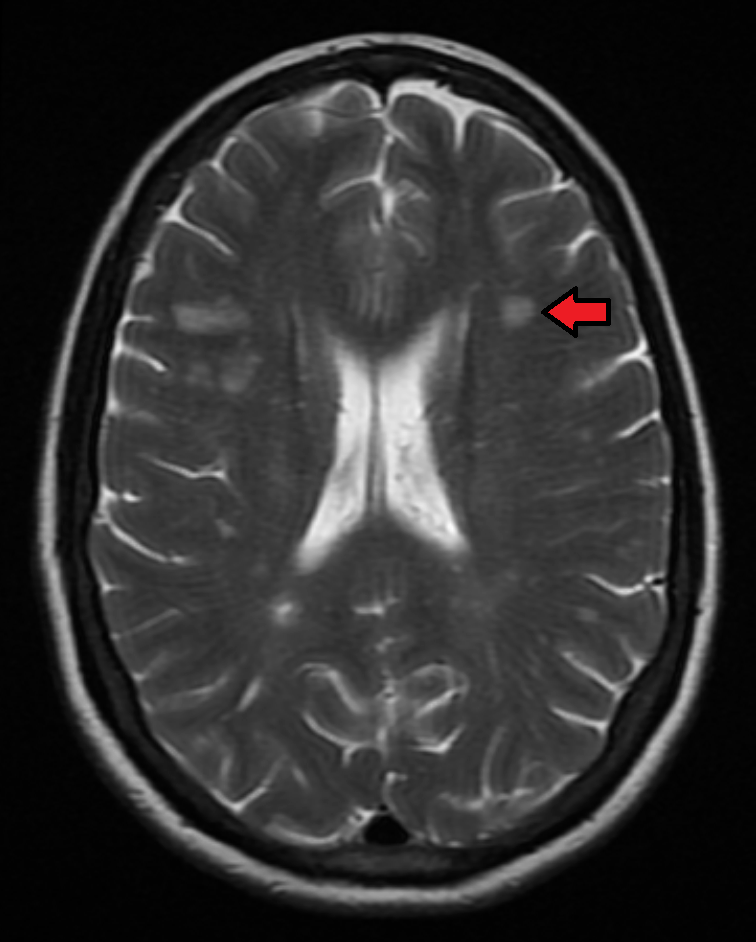
Characteristically, lamellar cytoplasmic inclusions are seen in brain macrophages, Schwann cells, Leydig cells, and adrenocortical cells. These lamellar inclusions consist of cholesterol esterified with VLCFAs. Periventricular demyelination is seen in the occipital region.
(II) Metabolic encephalopathies: These are caused by systemic illnesses that impair cerebral metabolism.
These conditions affect the functions of the neocortex and the ascending reticular activating system (from the brainstem), leading to changes in the level of consciousness. Presentations may include confusion, altered sensorium, small pupils, slow respiration, asterixis (flapping tremor), seizures, and coma.
(III) Multiple sclerosis or MS: This is a chronic, inflammatory, demyelinating disease of the CNS. It is more common in women of Northern European ancestry. MS is caused by a combination of factors, including genetic predisposition plus prior viral infection and/or environmental triggers, leading to autoimmune attack and destruction of the myelin sheath and oligodendrocytes.
Previous infections with EBV, HHV 6, Chlamydia pneumoniae, and HLA DR2 increase the risk of MS. It can be either type IV or type II hypersensitivity. Some studies have found that patients suffering from MS are deficient in linolenic acid.
| Type | Characteristics |
| Relapsing-remitting | Most common; flare ups followed by remission |
| Secondary progressive | Flare ups do not go into complete remission; worsens over period of time |
| Primary progressive | Symptoms continue to worsen from the beginning; no remissions or relapses; difficult to treat |
| Progressive -relapsing | Intermittent flare ups of worsening symptoms without remissions |
MS is diagnosed based on:
On biopsy, multiple discrete pink or gray areas with a rubbery texture are seen, showing loss of myelin and oligodendrocytes and an inflammatory exudate containing CD4+ T cells. Axons and neurons are preserved.
Clinical features include sensory disturbances (tingling, numbness, “pins and needles” sensation), fatigue, diplopia, vertigo, tremors, ataxia, numbness in limbs, optic neuritis, bladder incontinence, and constipation. Babinski sign is positive. Internuclear ophthalmoplegia may be present due to demyelination of the medial longitudinal fasciculus.
CSF shows normal glucose, increased proteins (especially gamma globulins and myelin basic protein [MBP]), and increased CD4+ T cells. CSF electrophoresis shows oligoclonal bands.
(IV) Central pontine myelinolysis (CPM): This is characterized by myelin destruction in the pons following rapid correction of hyponatremia. It typically presents 2-3 days after correction with altered sensorium, dysarthria, and dysphagia, followed by flaccid and later spastic quadriplegia. In severe cases, it can progress to “locked-in syndrome,” coma, and death.
Malnourished and alcoholic individuals are at greater risk of CPM. Microscopically, the lesion shows degeneration and loss of oligodendrocytes with preservation of axons.
Rapid correction of hyponatremia causes neurons to shrink and damages the blood-brain barrier. This leads to osmotic stress and activation of plasminogen, proteases, and cytokines, resulting in oligodendrocyte loss and demyelination.
(V) Guillain-Barre syndrome (acute inflammatory polyneuropathy or post-infective polyneuritis or GBS): This is a rapidly progressive, autoimmune polyneuritis that typically follows an infection of the gastrointestinal or respiratory tract. Common associated pathogens include Mycoplasma pneumoniae, Campylobacter jejuni, HIV, EBV, CMV, Zika, HEV, and influenza viruses.
It presents as a bilateral ascending paralysis: weakness begins in the feet and spreads upward to involve the arms and trunk. Symptoms may include tingling, “pins and needles” sensation, numbness, and muscle pain. Severe cases can involve respiratory paralysis and difficulty swallowing. “Glove and stocking” paresthesias are seen.
Autonomic imbalances (pulse and blood pressure variations and arrhythmias) may occur. Deep tendon reflexes are lost.
The mechanism involves molecular mimicry (sharing of epitopes) between myelin or the Schwann cell membrane and antecedent infectious agents, leading to an autoimmune response against peripheral nerves. Myelin loss from Schwann cells and axons of peripheral nerves is seen.
CSF examination shows albuminocytologic dissociation, meaning increased CSF protein with normal cell count and normal glucose levels.
Sign up for free to take 2 quiz questions on this topic