They are divided into four classes depending on the mechanism of action, as follows:
i) Class I or sodium channel blockers: They block fast sodium channels. This decreases the slope of phase 0 of the cardiac action potential and decreases the amplitude of the action potential. As a result, conduction velocity decreases and re-entry currents are blocked. They do not affect nodal tissues.
Class IA increases the effective refractory period (ERP). This group includes quinidine, procainamide, and disopyramide. Adverse effects include cinchonism (tinnitus), dizziness, blurred vision, and headache with quinidine, and a lupus-like syndrome with procainamide. Quinidine may enhance digitalis toxicity and precipitate Torsades de pointes in long QT syndrome. Class IA drugs also have anticholinergic adverse effects.
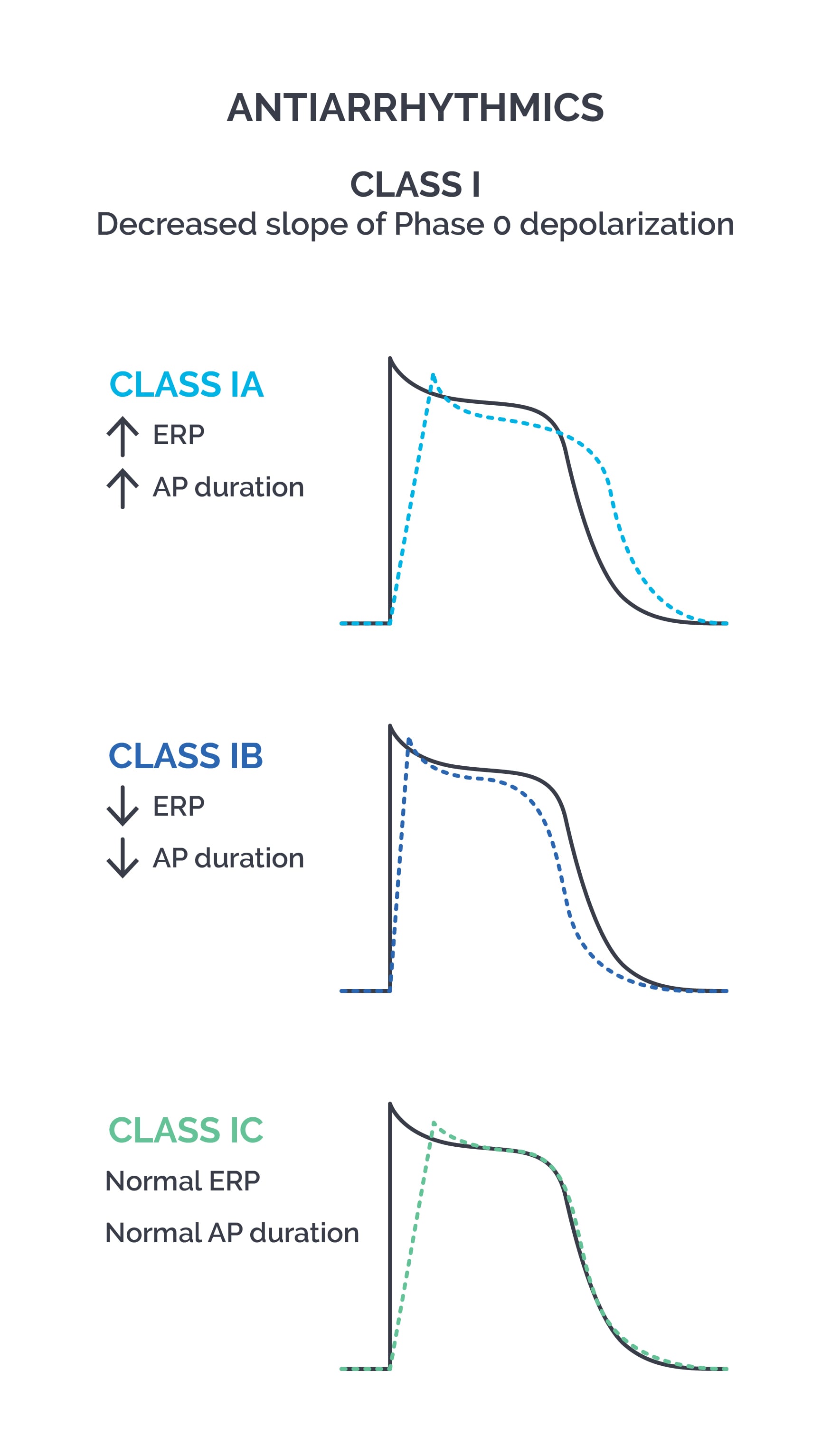
Class IB decreases the effective refractory period. This group includes lidocaine, tocainide, and mexiletine. Lidocaine and mexiletine have good efficacy in ischemic myocardium.
Class IC has no effect on the effective refractory period. This group includes flecainide, propafenone, and moricizine.
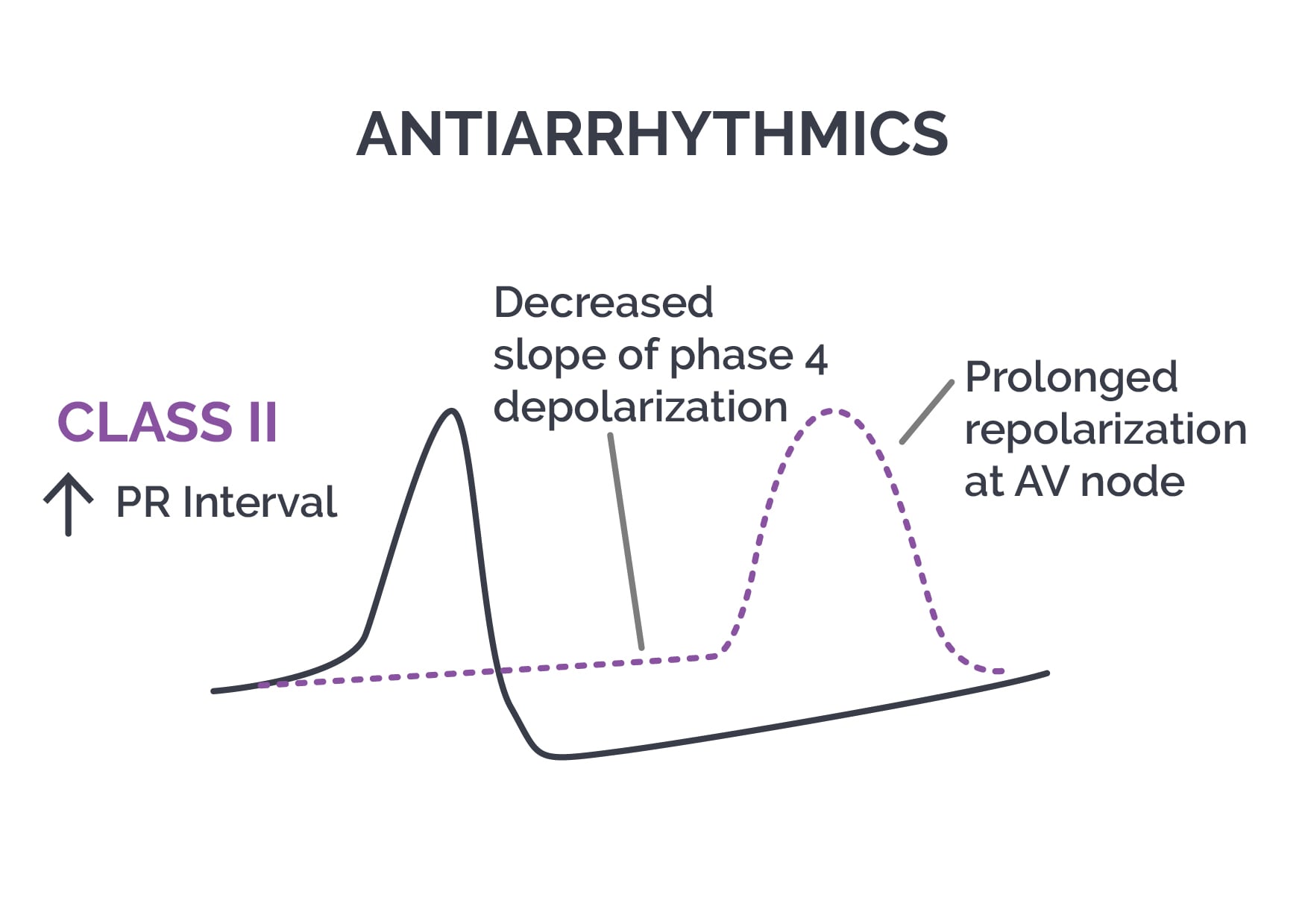
ii) Class II or beta blockers: Antiarrhythmic activity is caused by beta 1 receptor blockade and sympatholytic effects. These drugs decrease heart rate and conduction velocity, inhibit SA node pacemaker activity, increase the duration of the myocyte action potential, and increase ERP.
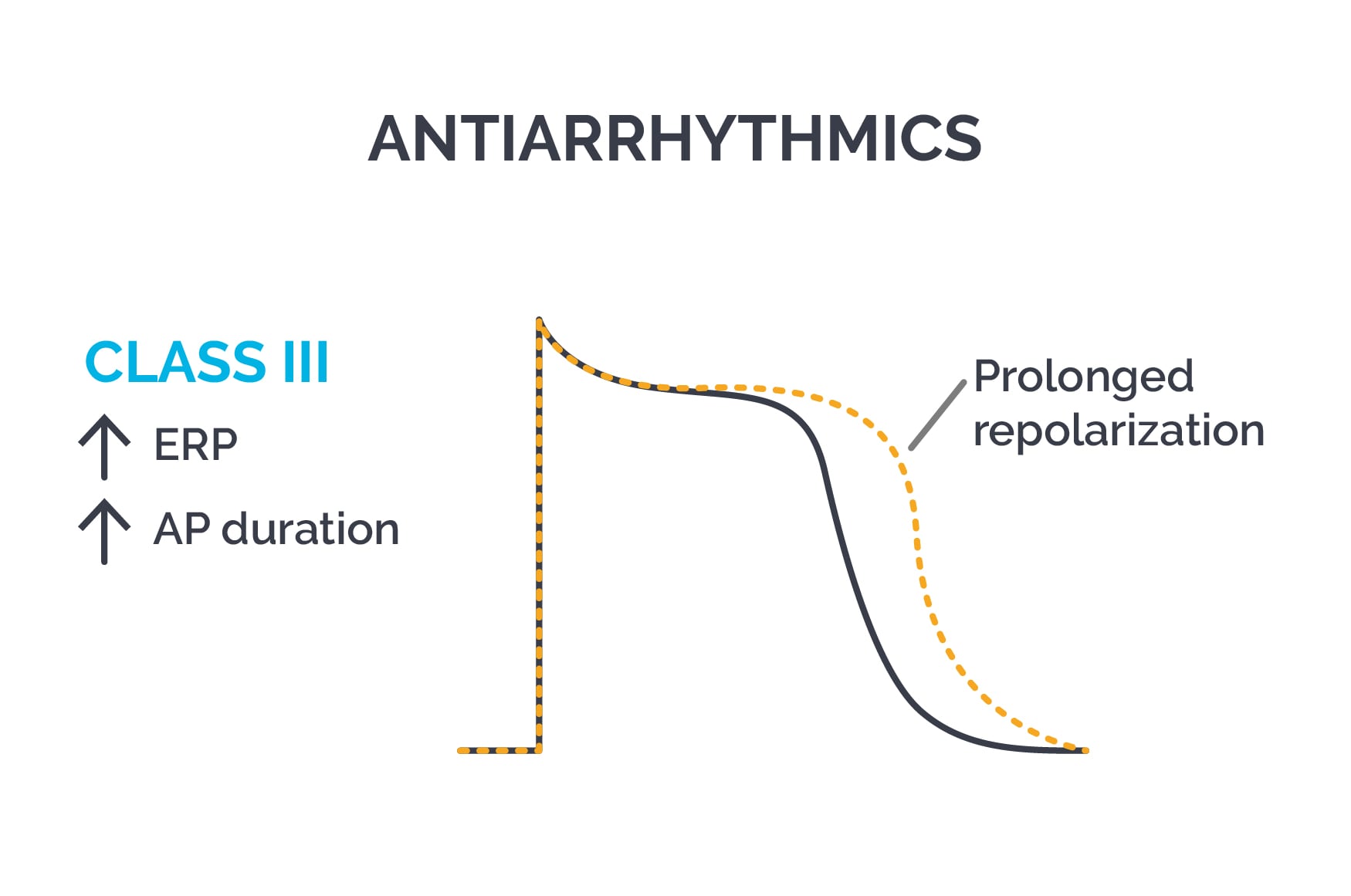
iii) Class III or potassium channel blockers: They block potassium channels, prolong phase 3 repolarization, increase the duration of the action potential, and increase ERP. They increase the QT interval and are effective in reentrant tachycardias. This class includes amiodarone, dronedarone, bretylium, sotalol, ibutilide, and dofetilide. Amiodarone is used in ventricular tachycardia, ventricular fibrillation, and atrial fibrillation. It has a long half life of up to 2 months and also has Class I, II, and IV effects. Pulmonary fibrosis and thyroid imbalance are serious adverse effects of amiodarone. Class III drugs may precipitate torsades de pointes.
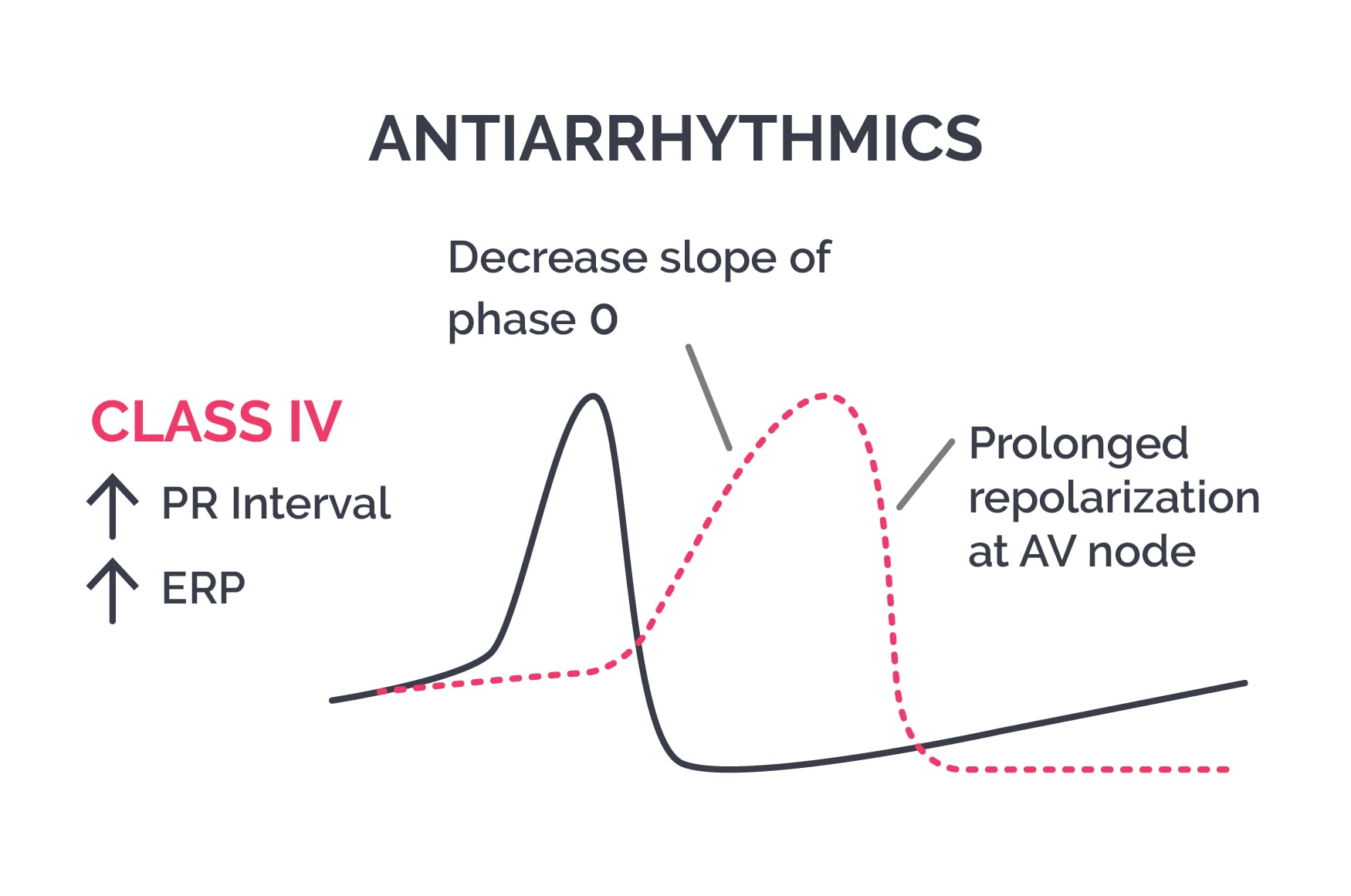
iv) Class IV or calcium channel blockers: They block L type calcium channels in nodal tissue, especially the AV node. This decreases conduction velocity, prolongs repolarization, and decreases firing rates of aberrant pacemakers. Verapamil and diltiazem are used.
Patients with sinus tachycardia are treated with beta blockers or calcium channel blockers when needed. In atrial flutter or fibrillation, ventricular rate is controlled with either digitalis, adenosine, Class IA, IC, II, III, or IV drugs. All these drugs, except digitalis, are also helpful in SVT. Atropine can be used in AV block. Ventricular tachycardia is treated with Class I, II, or III drugs.
v) Miscellaneous antiarrhythmics
Adenosine: It is a breakdown product of ATP, formed by the action of the enzyme 5’ nucleotidase. It is a purine nucleoside that binds to purinergic receptors and has two main effects on the CVS: vasodilation and slowing of heart rate and AV conduction. It has a half life of <10 seconds. Its antiarrhythmic effect occurs by binding to Gi coupled A1 receptors, opening K channels (causing hyperpolarization), decreasing cAMP, inhibiting L-type calcium channels, and inhibiting pacemaker current. This decreases the slope of phase 4 of the pacemaker action potential and can cause AV block. Its vasodilatory effect is due to binding the Gs coupled, type 2A adenosine receptor, which increases cAMP, activates K-atp channels, hyperpolarizes the smooth muscle membrane, inhibits myosin light chain kinase, and decreases intracellular calcium, leading to vasodilation.
Digitalis: It binds to and inhibits the Na/K ATPase pump. Related compounds include digoxin, digitoxin, and ouabain. This pump moves 3 Na out of the cell and brings in 2 K ions. Therefore, the Na/K ATPase pump is electrogenic and requires ATP. Digitalis inhibits the Na/K ATPase pump, which increases intracellular Na in the myocyte. This leads to accumulation of intracellular calcium via the Na-Ca exchanger system. More calcium is then released from the sarcoplasmic reticulum, causing positive inotropy (increased force of contraction).
Digitalis has a narrow therapeutic index, so plasma levels need to be monitored. Risk is increased because digitalis has a long half life. Certain drugs increase the toxicity of digoxin, including quinidine (displaces digoxin from binding sites and decreases renal clearance), calcium channel blockers, NSAIDS, amiodarone, and beta blockers. Toxicity is aggravated by hypokalemia, as seen with diuretic therapy. The dose of digitalis needs to be decreased in renal failure. Hypokalemia, hypercalcemia, and hypomagnesemia predispose to digoxin induced arrhythmias. Digitalis is contraindicated in WPW syndrome and AV block.
Digitalis toxicity presents with lethargy, fatigue, yellow halos, photophobia, blurred vision, nausea, vomiting, confusion, hallucinations, paresthesia, palpitations, bradycardia, etc. ECG shows downsloping ST segment depression, frequent PVCs with ventricular bigeminy and trigeminy, sinus bradycardia, AV block, ventricular ectopics, slow AF, atrial tachycardia with 2:1 block, ventricular tachycardia, etc. Treatment is with digoxin Fab fragments (which bind to the drug), correction of hypokalemia or hyperkalemia, hemodialysis if needed, and supportive therapy. In accidental or intentional ingestion of large doses of digitalis, gastric decontamination with activated charcoal is done within 6-8 hours after ingestion. Binding resins such as cholestyramine and colestipol decrease enterohepatic recycling of digitalis and enhance elimination.
Sign up for free to take 2 quiz questions on this topic