This family includes six important members: HSV 1 and 2, VZV, CMV, EBV, and HHV 8. They are known to cause latent infections and replicate in the nucleus, forming intranuclear inclusions.
It includes HSV 1 and HSV 2. Clinically, HSV 1 typically causes infections above the waist, while HSV 2 typically causes infections below the waist. HSV 1 is spread by direct contact or inhalation, while HSV 2 is an STD. After the initial infection, the virus becomes latent in ganglia:
It may reactivate due to stress, hormonal changes, fever, etc., and present as skin and mucosal lesions.
Clinical Features: HSV 1 commonly presents as umbilicated vesicles on the face, buttocks (napkin rash), or pustules on the finger (herpetic whitlow), which may or may not be accompanied by fever. In some children with eczema, it may present as a generalized eruption called eczema herpeticum. It may cause gingivostomatitis, keratoconjunctivitis, aseptic meningitis, and encephalitis. HSV 2 causes painful vesiculoulcerative lesions in the genital area with inguinal lymphadenopathy. Both types may cause neonatal herpes, which may present as encephalitis with or without skin lesions.

Laboratory diagnosis of HSV infections: The most commonly employed method is demonstration of the virus in scrapings from lesions in a Tzanck smear showing intranuclear inclusions and multinucleated giant cells. HSV induces fusion of adjacent cells, causing syncytium formation. Direct immunofluorescence can also be used. If needed, virus isolation is done in tissue culture, which will show giant cell and syncytium formation. Antibodies can be detected by neutralization tests, CFT, ELISA, RIA, and haemagglutination tests. Neonatal herpes is diagnosed by PCR or viral culture.

It is the causative agent of chicken pox and herpes zoster. Infection is spread by respiratory droplets and direct contact with vesicles. After the initial infection, the virus becomes latent in the dorsal root ganglia. It may reactivate when immunity is low or after local trauma.
Clinical features: The vesicles appear in crops, first on the trunk, and then spread to the face, limbs, and buccal mucosa in a centripetal distribution. Fever precedes the rash. At one time, you can see rashes in various stages ranging from macule, papule, vesicle, pustule, and scab. In adults, it may cause life-threatening encephalitis and pneumonia. It has also been associated with Reye’s syndrome. Herpes zoster presents with a prodrome of fever and severe neuritic pain, followed by a typical rash in a dermatomal distribution. Disseminated zoster can occur in immunocompromised persons. It may be complicated by post-herpetic neuralgia.

Laboratory diagnosis of varicella infections: A Tzanck smear will show multinucleated giant cells, syncytium formation, and intranuclear inclusions. Immunofluorescence can be used to detect intranuclear viral antigens. Serological tests for antibodies include ELISA, CFT, immunofluorescence, and CIEP. The virus can be grown in Vero cells, human fibroblast, or amnion culture.
It is the largest Herpesvirus. It is named as such because infected cells are greatly enlarged. The virus prevents infected cells from displaying viral antigens along with Class I MHC by blocking assembly of viral peptides to MHC molecules and also by interfering with translation of MHC I proteins by the cell. When cell mediated immunity is down, the virus can cause disseminated infections. CMV can become latent in the leukocytes and kidneys.
Clinical features: It causes heterophile negative infectious mononucleosis. It presents as malaise, myalgia, fever, lymphocytosis with abnormal lymphocytes, lymphadenopathy, and splenomegaly. It may cause pneumonia, hepatitis, cytopenia, encephalitis, retinitis, and colitis in immunocompromised individuals. Congenital infection is also called cytomegalic inclusion disease. It is characterized by hepatosplenomegaly, jaundice, thrombocytopenia, hemolytic anemia, microcephaly, chorioretinitis, seizures, and deafness. It may lead to mental retardation. Infection is most severe when acquired during the first trimester.
Laboratory diagnosis of CMV infections: Demonstration of typical “owl’s eye” intranuclear inclusions in enlarged cells is characteristic. DNA hybridization or electron microscopy can be used to view the virus. Pp65 from the CMV capsid can be detected by immunofluorescence. It can be isolated in human fibroblast culture. Antibody detection methods are like for VZV. Urine samples can also be used for diagnosis.
EBV has affinity for CR2/D21 receptors on human lymphocytes, which helps in pathogenicity. It becomes latent in the B lymphocytes. It causes transformation of T lymphocytes to atypical lymphocytes. Disease is spread by saliva and kissing, hence the nickname “kissing disease”.
Clinical features: It causes a heterophile positive infectious mononucleosis. It may cause exudative or non exudative pharyngitis with palatal petechiae. The exudative type may be confused with streptococcal pharyngitis. Diagnosis is complicated by the fact that patients infected with EBV may be carriers of streptococci as well. Look for uvular edema, which is specific to EBV. Other symptoms are sore throat, high fever, and lymphadenopathy. Splenomegaly with splenic rupture can occur, so patients should avoid contact sports. Hepatitis and encephalitis can occur.
EBV is associated with Burkitt’s lymphoma, nasopharyngeal carcinoma, lymphomas, and oral hairy leukoplakia.
Laboratory diagnosis of EBV infections: Absolute lymphocytosis with atypical lymphocytes is seen; these are cytotoxic T cells with vacuolated cytoplasm and a lobed nucleus. The Monospot test is commonly done to detect heterophile antibodies. Antibodies to the viral capsid antigens (VCA) are used to diagnose difficult cases. IgM VCA is used in early disease, while IgG VCA is used in late disease diagnosis. Rarely, antibodies to early antigens (EA) or nuclear antigens (EBNA) are used. Nucleic acid hybridization is a sensitive test. Other antibody tests are CFT, ELISA, gel diffusion, and indirect immunofluorescence. Culture is not preferred as it is technically difficult.
This fairly recently isolated virus has two types, A and B, with type B causing most infections. Viral DNA gets integrated with the host genome and may be vertically transmitted. It causes roseola infantum, also called Sixth’s disease or exanthem subitum. It is a self-limiting disease seen in children under 2 years of age, presenting as a high fever for 3-5 days followed by an erythematous maculopapular rash. The rash starts at the trunk and spreads centrifugally to the face and limbs, blanches on pressure, and usually fades in 1-2 days. Febrile seizures may be caused. It causes life-threatening encephalitis, hepatitis, and lymphadenopathy in immunocompromised. It has been associated with chronic fatigue syndrome and multiple sclerosis, but definitive evidence is lacking.
Diagnosis is made by immunohistochemical staining of samples and/or a fourfold rise in antibody titres. PCR is controversial as test results are difficult to interpret. [ send us your answers ] . Cell culture can be done mainly for research purposes.
It is the causative agent of Kaposi’s sarcoma. It is an STD. Infection is primarily seen in immunocompromised patients, as in AIDS and organ transplants. Kaposi’s sarcoma is a malignant proliferation of endothelial cells which, on gross appearance, is purplish (think lots of blood vessels), with multiple nodular lesions on skin and mucosa. Inactivation of the Rb tumor suppressor gene is the mechanism of oncogenesis. It has also been associated with Castleman’s disease and primary effusion lymphoma. Biopsy showing highly vascular lesions with spindle-shaped cells is a means of diagnosis.
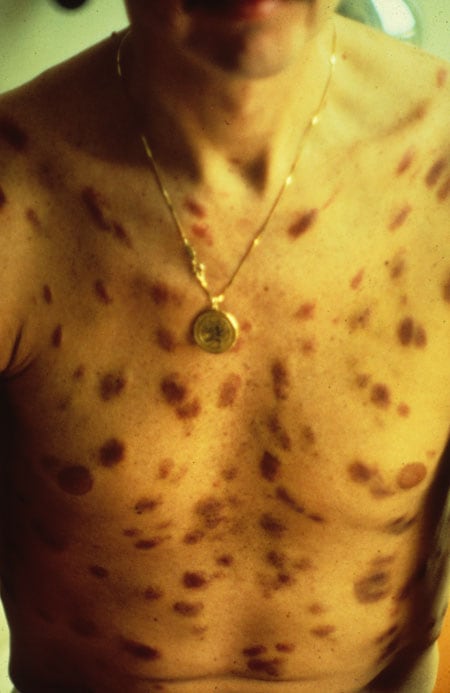
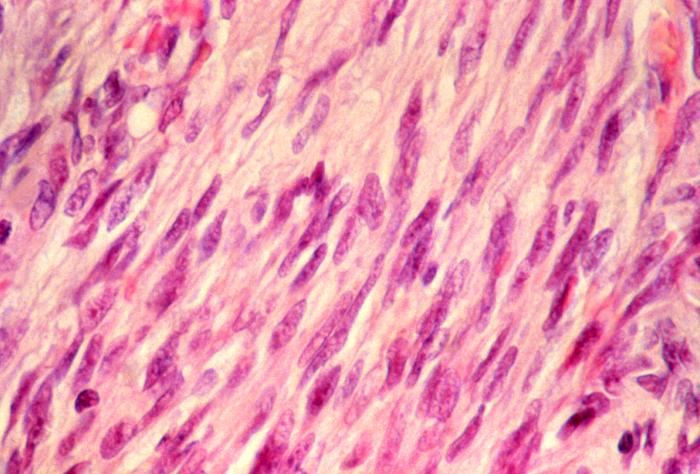
This photomicrograph reveals some histopathologic changes in a Kaposi’s sarcoma lesion tissue sample. This skin biopsy featured the usual dermal infiltrate of spindle-shaped cells representing young fibroblasts.
Sign up for free to take 5 quiz questions on this topic