Most prescriptions are paper, also known as written prescriptions. Traditionally, paper prescriptions are manually written and signed by the prescriber. A paper prescription may be printed and then manually signed by the prescriber. Some prescriptions are telephonic or verbal, where the prescriber or an assigned agent calls in a prescription to the pharmacy. Some prescriptions can be transmitted as facsimiles. Sometimes, prescriptions are faxed. However, many prescribers are increasingly using E-prescriptions. Sending a prescription electronically is known as E-prescribing. In inter-pharmacy transfers, prescriptions are transferred electronically between two pharmacies.
Prescription intake is one of the responsibilities of the pharmacy technician. When the pharmacy receives a prescription, it is tracked using prescription origin codes (POC). The prescription origin codes are as follows:
| POC | Meaning |
| 0 | Unknown: This is used when the method of receiving the original prescription is unknown, which may be the case in a transferred prescription. |
| 1 | Written prescription via paper, which includes computer-printed prescriptions that a physician signs as well as traditional prescription forms |
| 2 | Telephonic prescription |
| 3 | E-prescriptions |
| 4 | Facsimile prescription obtained via fax transmission |
All prescriptions must be checked for accuracy and completeness. Tamper-resistant prescription forms are a requirement for prescribing controlled substances.
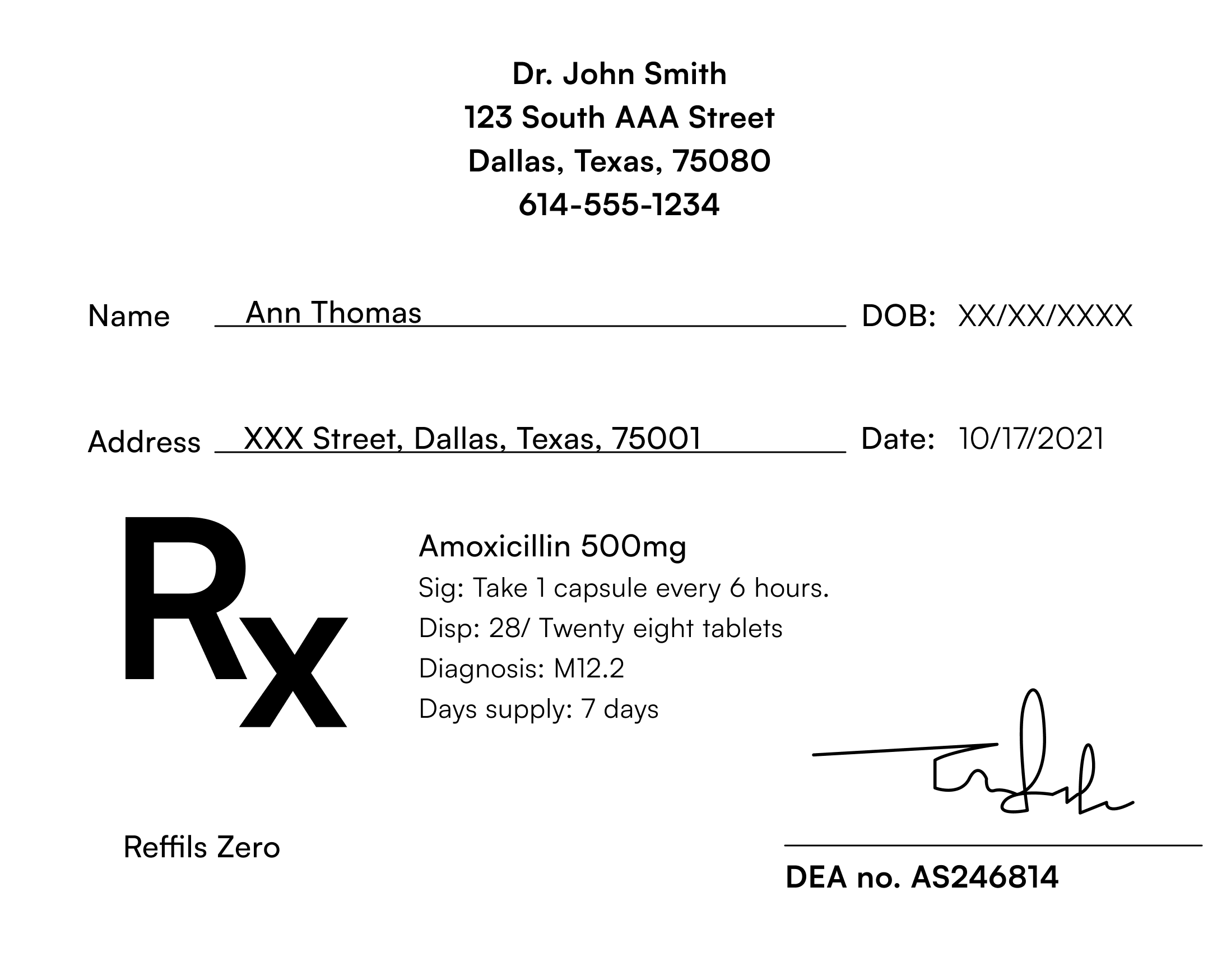
Parts of a prescription are as follows:
“Dispense As Written” codes or product selection codes indicate what type of product - brand name or generic substitution is allowed. The DAW code is found on the prescription.
| DAW code | Meaning |
| 0 | No product selection indicated; default |
| 1 | Substitution not allowed by prescriber |
| 2 | Substitution allowed - patient-requested product dispensed; used when a patient requests a specific brand of drug |
| 3 | Substitution allowed - pharmacist selected product dispensed; used when the pharmacist determines that the brand product should be dispensed. |
| 4 | Substitution allowed - generic drug not in stock when the pharmacist dispenses brand name drug due to lack of availability of generic drug. |
| 5 | Substitution allowed - brand drug dispensed as generic |
Data from the prescription is recorded in the pharmacy database. In addition to the details on the prescription, additional information like drug allergies, the patient’s contact number, current insurance information, and the time for picking up medications (community pharmacy) is also recorded. Controlled substances also need a government-issued ID verification.
How to calculate days’ supply: Days supply is the estimate of how many days a prescription is intended to last and is computed by dividing the number of doses in the prescription by
the number of doses per day. Calculating a day’s supply will depend on the dosage form, such as tablets, suspensions, injectables, etc.
Calculating days’ supply for tablets and capsules: For example, the prescription states, “Tablet Amoxicillin 500 mg tid for 7 days # 21 tablets”. The days’ supply will be calculated as follows -
Days’ supply = Number of doses in the prescription / Number of doses per day = 21/3 = 7 days supply
Calculating days’ supply for liquids: For example, if the prescription states, “Amoxicillin 400 mg/5ml 200 ml, 2 tsp q12h x 10 days”, it means a total of 200 ml has to be dispensed. Convert the teaspoons to ml, 1 tsp = 5 ml, so that each dose will be 10 ml; the daily dose will be 20 ml.
Days’ supply = 200 ml/20 ml = 10 days’ supply.
PRN dosing: For any medication, when the prescriber states that it can be used “as needed” or “prn,” we have to calculate the highest dose and shortest interval. For example, the prescription states, “ Tablet Ibuprofen 400 mg #30 1-2 tabs po q6-8h prn for pain.” The highest dose is 2 tablets, and the shortest interval is every 6 hours. The decimals have to be rounded off.
Days’ supply = 30/2x4 = 30/8 = 3.75, about 4 days’ supply.
Calculating days’ supply for ointments and creams: For creams and ointments, a single dose ranges from 0.5-1 gram. The dose also varies depending on the size of the affected area. Sometimes, prescriptions may mention doses in finger-tip units. 1 finger-tip unit (FTU) equals 0.5 gram .1 FTU can be applied over an area that corresponds to double the size of the flat of a hand.
For example, the prescription states, “Desonide 0.05% ointment, apply thin film tid, dispense 30 g.”
In this case, 0.5 g is a better dose indicator, as the instruction is to apply a thin film.
Days’ supply = 30 g/1.5 g = 20.
Calculating days’ supply for inhalers and sprays: The package of inhalers and sprays mentions the total number of inhalations, actuations, or metered doses per container. Each dose typically is 1-2 puffs or sprays and is mentioned on the prescription. For example, the prescription states, “Advair 125-25 MCG inhaler, 2 sprays qd x 1 month,” and the package states 60 metered actuations.
Days’ supply = 60/2 = 30.

Calculating days’ supply for Insulin: Insulin is packaged in vials, pens, syringes, and pumps. Insulin dosing is stated as the number of “Units’’ of insulin. Standard insulin contains 100 units in 1 mL. This is also called U-100 insulin. Insulin syringes are marked as 1-2 units per small marking depending on the syringe size e.g., 50 U versus 100 U syringe. More concentrated insulins, such as U-300 and U-500, have recently become available. Each insulin package may have a single multidose vial or multiple vials or pens. To calculate the days’ supply, calculate the total number of Insulin units in the package.
For example, 1 package of Humalog carries one 10 ml vial of strength 100 U/ml. Hence, 1 package has a total of 10 x 100 = 1000 Units of insulin. Similarly, one package of Humulin N Kwikpen has five 3 ml pens of strength 100 U/ml. Hence, the total dose per package is 100 x 3 x 5 = 1500 units. Dividing the total dose into units by the number of units to be taken each day will give the days’ supply of Insulin. The days’ supply must never exceed the expiration date after opening. If the days’ supply calculation yields a decimal number, then drop the decimal, e.g., convert 25.45 to 25.
For example, a prescription for Humulin U-100 states, “ Administer 50 U subcutaneously 30 mins before breakfast and dinner.” Considering it has a single 10 ml vial containing 100 U/ml, the total dose in the package is 1000 units.
Days’ supply = 1000 / 50+50 = 1000/100 = 10 days’.
Calculating days’ supply for injectables: It is similar to insulin, except that instead of Units, we will consider milliliters (ml). Divide the total number of milliliters of the product available in vials, ampules, or syringes by the number of milliliter daily doses.
For example, if the prescription for a 5 ml package of injection triamcinolone 40 mg/ml states, “Inject 20 mg im q12h.” The total daily dose is 40 mg, which equals 1 ml/day.
Daily dose = 5 ml/1 ml = 5 days.
Calculating the days’ supply for eye and ear drops: A standard dropper delivers about 20 drops/ml or 20 gtt/ml. The days’ supply is calculated by dividing the total number of drops dispensed by the number of drops required for each dose.
For example, the Sig code for Latanoprost eye drop 0.005% dispensed as a 2.5 ml bottle states “1 gtt ou bid”.
2.5 ml = 2.5 x 20 = 50 drops total
Daily dose = 4 drops per day (includes both eyes)
Days’ supply = total number of drops dispensed / daily dose in drops = 50/4 =12.5 days
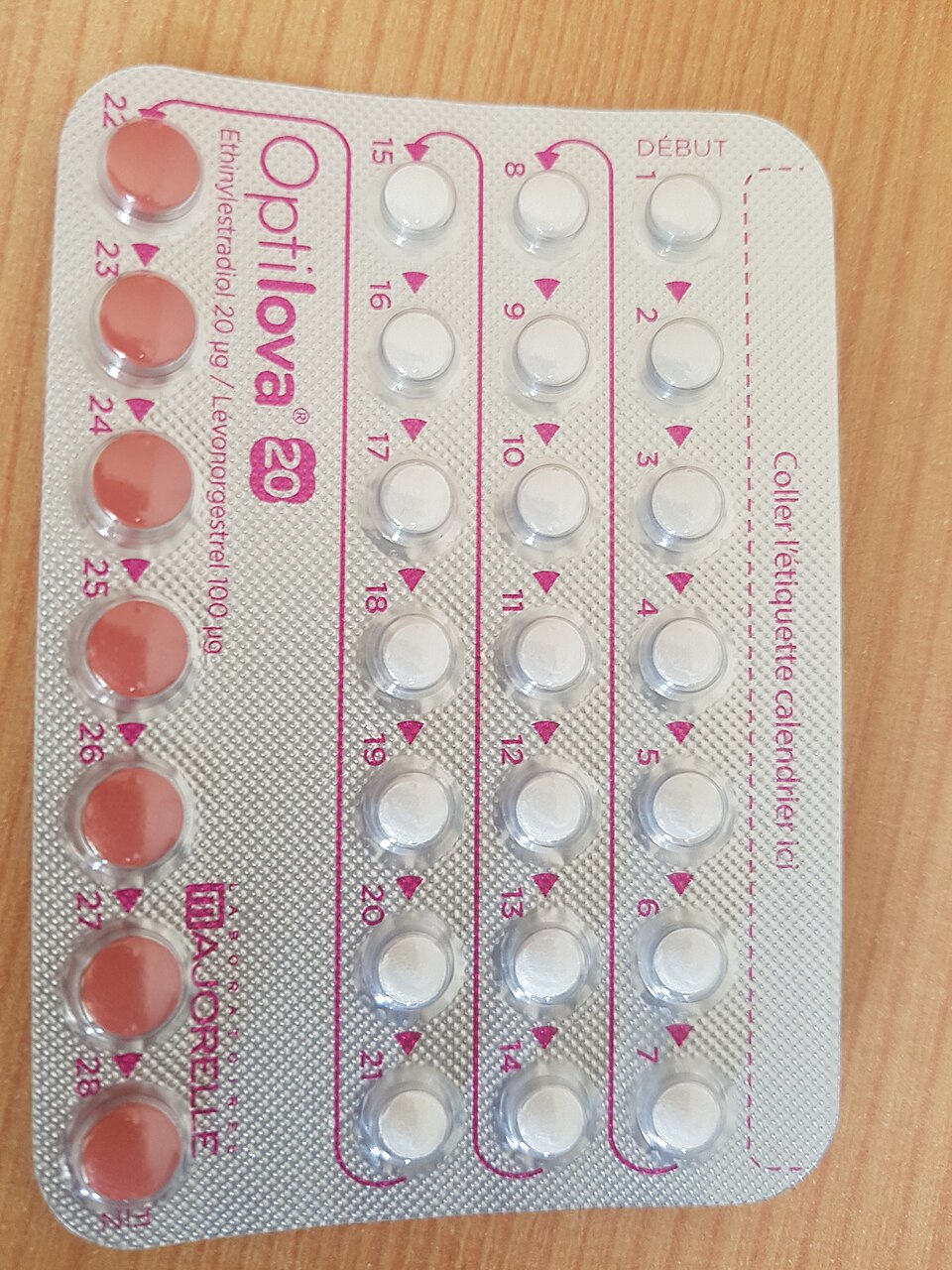
Days’ supply for packs: Certain medications like birth control pills, steroid tablets, and certain antibiotics like Azithromycin are dispensed as readymade packets. Each packet has detailed instructions stating the days of supply. For example Z pack for Azithromycin states how many tablets to take on days 1 to 5. Hence, days’ supply will be 5 days. Similarly, birth control pills come in 21-day or 28-day packets; hence, days’ supply will be 21 or 28 days per packet, respectively.

Refills: The number of refills is written on the prescription. Even though a prescription may include 90-day or 3-month supply, insurance may only allow to fill for 30 days at one time. It also depends on the medication type. If refilled too early, insurance will reject it. In special circumstances like traveling abroad, an early refill may be requested. Many insurances need prior approval for early refills. A new prescription is required if the prescription is over a year old. Partial fill is done when the pharmacy doesn’t have adequate stock to fill a prescription or refill. A 2-5 day supply of medication can be dispensed to the patient until the pharmacy can fill the balance of the prescription.
State and federal laws dictate how controlled substances are refilled. Schedule II medications cannot be refilled. Instead, they need a new prescription for every fill. Generally, the prescription has a validity of six months. Schedule III and IV cannot be refilled after six months or five times, whichever is earlier. Generally, prescribers write sequential prescriptions for Schedule II medications, with a “Do not fill until” date on each prescription. Schedule V medications may be written for up to 1 year, although many states limit this to 6 months.
Legend medications: A legend drug is a medication that requires a prescription. A legend drug can be dispensed upon receipt of a prescription from a licensed healthcare provider. It is labeled with the legend “Rx” only. On the other hand, OTC or over the counter medications are also known as “non-legend” medications as they do not need a prescription.
Once the prescription is received, the order must be entered into the pharmacy management system. Details from the prescription, as discussed above in prescription intake, are entered into the system along with a copy of the prescription itself. Additional information like scheduling a pickup time or delivery services, updating allergy and contact information, and checking for drug inventory status is done at this stage to avoid potential delays in filling and processing medications.
The correct NDC number needs to be picked at this stage. NDCs change with manufacturers, dosage forms, strengths, and packaging. So even the same active ingredient, such as Prednisone, will have multiple NDC numbers.
Pharmacy benefit managers (PBM) serve as intermediaries between the pharmacy, drug manufacturers and insurance companies. They are closely associated with formulary design, utilization management, price negotiation, pharmacy network formation, and mail-order pharmacy services. The three largest PBMs are Express Scripts, OptumRx, and CVS Caremark.
Sign up for free to take 19 quiz questions on this topic