It’s a leading nosocomial pathogen and is associated with high mortality in sepsis. It’s resistant to many antibiotics and can be very difficult to eradicate from the environment.
P. aeruginosa produces several virulence factors, including enzymes, exotoxin, endotoxin, and a bluish-green pigment called pyocyanin. It also produces abundant glycocalyx (biofilm) or a slime layer, which helps it persist both in the body and in the environment. These biofilms are especially common in the lungs of patients with cystic fibrosis; when cultured, these strains typically produce mucoid colonies.
It can cause wound infections (especially burn wounds), ventilator-associated pneumonia, UTIs, malignant otitis externa, hot tub folliculitis, and osteochondritis following puncture wounds in the foot. Rarely, patients with Pseudomonas bacteremia can develop ecthyma gangrenosum, in which the skin develops hemorrhagic bullae that ulcerate and form black eschars.
In practice, any Gram-negative bacillus that is oxidase positive should be considered Pseudomonas first, especially in the clinical scenarios listed above. Additional clues include:
During outbreaks, bacteriophage typing or pyocin typing can be used to help locate the source and guide preventive measures.
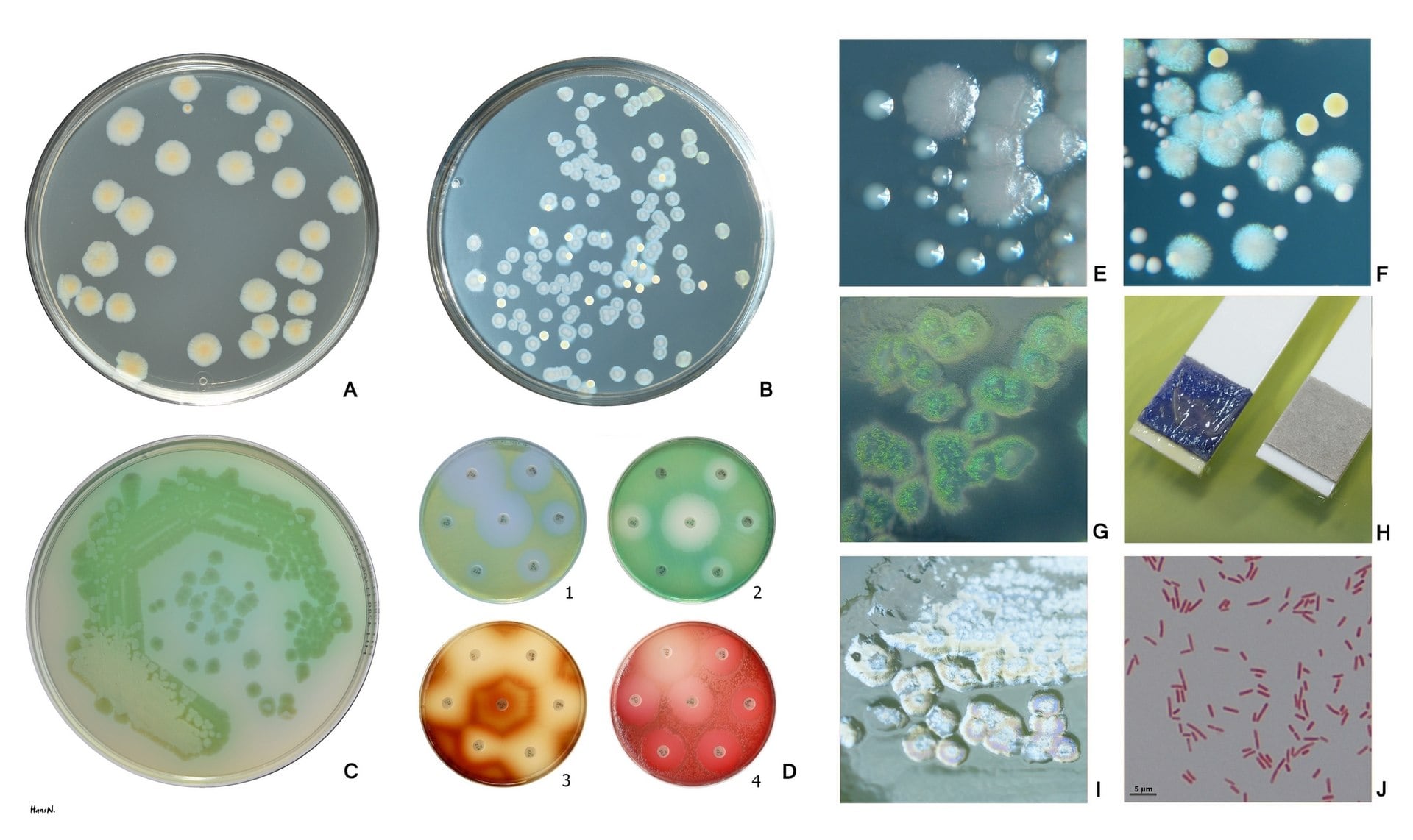
Pseudomonas aeruginosa is a nonfastidious, Gram-negative (Fig. J), oxidase positive (Fig. H), nonfermenting rod. P. aeruginosa produces pyoverdin, a water-soluble yellow-green pigment (Fig. A, C, D1, D2). Many P. aeruginosa strains also produce the blue pigment pyocyanin (Fig. B, F). When pyoverdin combines with pyocyanin, the bright green color characteristic of P. aeruginosa is created (Fig. C). Some strains rarely produce other pigments: brown pyomelanin (D3) or red pyorubrin (D4). For the isolation and presumptive identification from clinical and environmental samples a selective agar containing cetrimide can be used (Fig. G). Fig. A, B Trypticase soy agar (B: P.aeruginosa + S.aureus), Fig. C, D, I Mueller-Hinton agar Fig. E Larger colonies of P. aeruginosa and smaller colonies of Enterococcus faecalis on tripticase soy agar. Reflected light. Fig. F Bluish colonies of P. aeruginosa, yellow colonies of S. aureus and white colonies of Enterococcus faecalis on trypticase soy agar. Fig. I Plaques are frequently found in freshly isolated strains, especially in the area of confluent growth. In some strains these are caused by phage, in others by bacteriocins.
Sign up for free to take 1 quiz question on this topic