The factors important in pathogenicity are pili (for initial adhesion to cells), enterotoxins (heat stable and heat labile toxins), endotoxin (as in all Gram negative bacteria), and capsule (seen in invasive strains causing systemic infections and septicaemia).
Heat labile toxin: Like cholera toxin and the enterotoxin of Bacillus cereus, the heat labile toxin of E.coli causes ADP ribosylation and activation of Gs. This stimulates adenylate cyclase, increasing cAMP. The result is loss of Na, Cl, and water from intestinal cells, which presents as watery diarrhea. The toxin has two subunits, A and B:
Heat stable toxin: This is a polypeptide not inactivated by boiling for 30 minutes. It stimulates guanylate cyclase to increase cGMP, inhibiting the reabsorption of sodium and causing diarrhoea.
Verotoxin or Shiga-like toxin: This toxin is produced by EHEC (enterohemorrhagic E.coli) or STEC, especially strains such as E. coli O 157:H7. It inactivates protein synthesis by removing adenine from 28 S rRNA. It binds to receptors on the kidney and the endothelium of small vessels, causing hemolytic uremic syndrome and bloody diarrhea.
E.coli is a common cause of UTI and diarrhea.
UTI: E.coli is the leading cause of community acquired UTI. It presents as dysuria (pain and burning sensation during micturition), increased frequency, and rarely fever. Pili help the bacteria adhere to the urothelium and cause UTI. Some strains carrying the “K” antigen are also prone to cause UTI.
Diarrhea: Five types of E.coli cause diarrhea and/or dysentery (blood in stools). These are as follows:
EPEC (Enteropathogenic E.coli) - Seen in cases of diarrhea in children. Causes disruption of the brush border in the small intestine.
ETEC (Enterotoxigenic E.coli) - Cause of “traveller’s diarrhea”. Produces heat labile and heat stable toxins.
EIEC (Enteroinvasive E.coli) - Causes bloody stools due to invasion of the intestinal mucosa. It is peculiar in being non lactose fermenting and non motile. Keep this in mind in the differential of bloody diarrhea (dysentery).
EHEC (Enterohemorrhagic E.coli) - New terminology is STEC (shiga toxin producing E.coli). It may cause mild diarrhea to severe HUS, especially in small children, older adults, and immunodeficient individuals. Common implicated foods include raw (or undercooked) meat, lettuce, alfalfa sprouts, salami, or raw (unpasteurized) milk, juice, or cider. E.coli O157 diarrhea should NOT be treated with antibiotics, especially beta lactams and fluoroquinolones, as they have been shown to be associated with the development of HUS.
EAEC (Enteroaggregative E.coli) - Causes diarrhea due to production of heat stable enterotoxin.
Other infections caused by E.coli include meningitis and sepsis in infants and older adults, peritonitis, and wound infections.
Samples include urine, stool, blood, CSF, wound discharge, etc., depending on the clinical findings. Isolation by culture is not essential, since empiric treatment is typically started based on clinical features and history alone. Culture is important in cases showing resistance to antibiotics, septicaemia, meningitis, and suspected E.coli O 157 diarrhea.
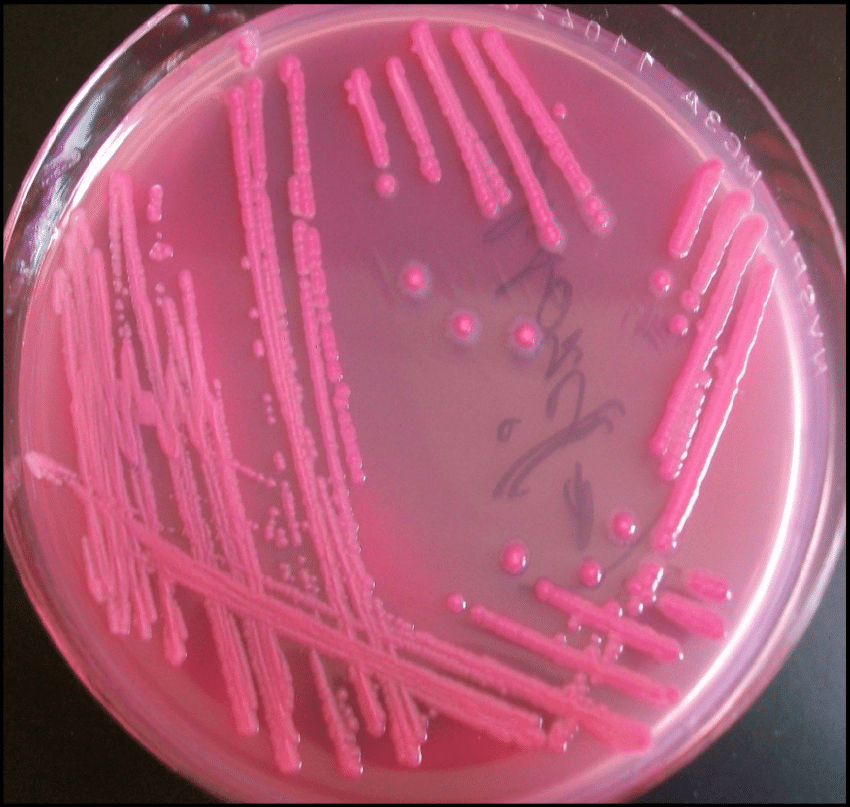
Gram stain shows Gram negative bacilli. MacConkey’s agar shows pink lactose fermenting colonies, except in EIEC. EMB agar shows colonies with a green metallic sheen. E.coli O 157 H7 can be identified by its inability to ferment sorbitol, which is characteristic.
Sign up for free to take 1 quiz question on this topic