Hypersensitivity: Hypersensitivity is an exaggerated immune response to an otherwise innocuous antigen. This immune response can lead to a disease state, especially when it becomes chronic or repetitive. Based on pathophysiology, hypersensitivity reactions are classified as follows:
Type I: Type I hypersensitivity is mediated by IgE. Allergens are antigens that trigger a type I hypersensitivity response in susceptible individuals by driving a predominantly Th2 immune response.
On initial exposure to an allergen:
On subsequent exposure:
Mast cell granules contain preformed enzymes (tryptase, cathepsin, carboxypeptidase) and inflammatory mediators (histamine, heparin). After activation, mast cells also release cytokines, chemokines, and lipid mediators such as IL4, IL13, TNF alpha, MIP, leukotrienes C4, D4, and E4, and platelet activating factor. The result is a sustained inflammatory response with:
Mast cell degranulation leads to characteristic physiologic effects:
Clinical features depend on where the inflammatory response occurs (for example, nasal mucosa in allergic rhinitis or bronchioles in asthma).
Eosinophils also contribute to tissue injury by releasing enzymes, cytokines, chemokines, and lipid mediators such as major basic protein, peroxidases, collagenases, eosinophil cationic protein, neurotoxin, IL3, 5, 8, PAF, and leukotrienes C4, D4, and E4. This contributes to tissue damage. Basophils release histamine and IL4.
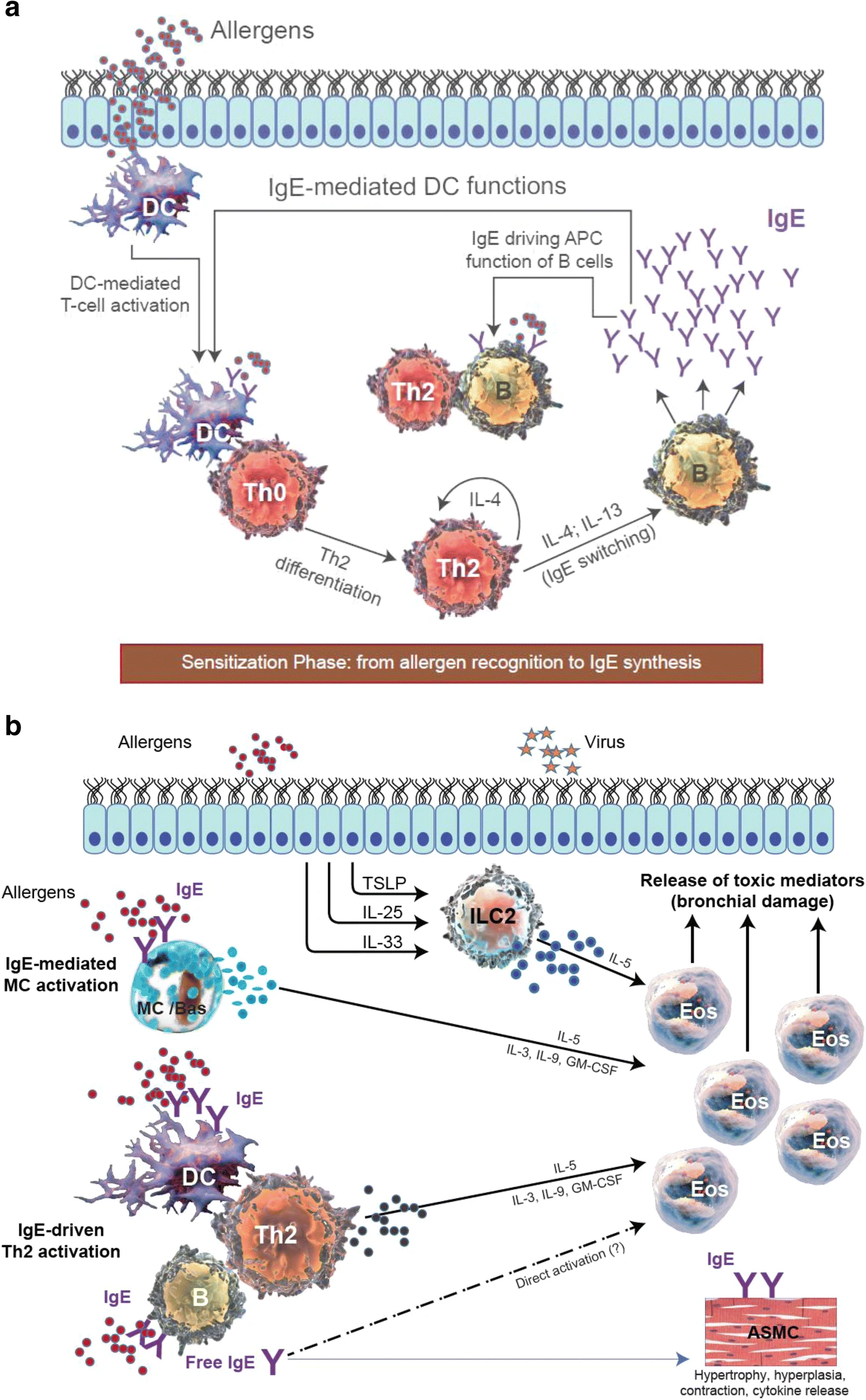
IgE-mediated responses occur in two phases: an immediate response followed by a delayed response.
| Route of exposure to allergen | Manifestations |
| Inhalation | Allergic rhinitis, asthma |
| Intravenous | Anaphylaxis |
| Subcutaneous | Wheal and flare reactions |
| Ingestion | Vomiting, diarrhea, may cause urticaria and anaphylaxis after absorption |
| Type | Features |
| Atopy | Tendency of exaggerated response to common environmental allergens; genetic predisposition; high levels of IgE and eosinophils; increased risk of allergic diseases like asthma, hay fever etc. |
| Anaphylaxis | Life threatening syndrome caused by disseminated mast cell activation; presents with shock, bronchoconstriction, epiglottic swelling; seen in the presence of preformed IgE to drugs like penicillin, insect bites or venom, peanuts, brazil nuts,shellfish |
| Allergic rhinitis | Results from the activation of mast cells in the nasal mucosa by inhaled allergens like pollen; manifests as nasal itching, rhinorrhea, sneezing, nasal blockage; eosinophils are present in the nasal discharge; |
| Allergic asthma | Results from mast cell activation in the lower airways; presents with dyspnea, bronchoconstriction, increased mucus and fluid discharge, airway hyperresponsiveness to environmental pollutants like cigarette smoke, sulfur dioxide; chronic inflammation with airway damage may occur; attacks may be exacerbated by viral respiratory tract infections |
| Urticaria (hives) | Ingested allergens may be absorbed into the bloodstream, reach the skin and activate allergen-specific mast cells in the skin to cause urticaria or hives, lesions are itchy, red papules; chronic urticaria is an autoimmune disorder caused by antibodies to FcεRI receptor |
| Eczema or atopic dermatitis | Chronic, relapsing inflammatory disease of the skin, first appears in early childhood, 25% cases progress to adult atopic dermatitis; increased risk of asthma and hay fever; familial history of allergy, atopy; filaggrin gene mutations may be seen; parakeratosis and hyperkeratosis seen; presents as itchy, erythematous, vesicular, maculopapular rash, with oozing and crusting; characteristically seen in flexures of the elbows and knees in children and face, scalp and extensor surfaces of the arms and legs in infants; common locations in adults include face, neck, hands |
Type II or cytotoxic: Type II hypersensitivity is also called antibody-mediated hypersensitivity. It is mediated by IgG or IgM produced in response to cell surface or matrix antigens. Antibody-bound cells are then cleared by Fc receptor-mediated phagocytosis by NK cells and macrophages in the spleen.
It is seen in drug-induced hemolytic anemia and thrombocytopenia with penicillin, quinidine, and methyldopa; some transplant rejections; Goodpasture’s syndrome; and in ADCC (antibody dependent cell mediated cytotoxicity). In complement-dependent type II hypersensitivity, antigen-antibody complexes activate complement, leading to cell lysis and tissue damage.
In some cases, antibodies are directed against receptors, for example:
Type III: Type III hypersensitivity is seen with soluble antigens and is mediated by IgG. Antigen-antibody complexes deposit in blood vessels and locally in tissues, causing type III hypersensitivity reactions.
Arthus reaction is a local type III reaction. It occurs when an antigen is injected into the dermis and reacts with preformed IgG, leading to complement activation, binding to Fc receptors on leukocytes (Fcgamma on eosinophils), and a local inflammatory response.
Serum sickness is a systemic type III hypersensitivity reaction. In the modern era, it is more commonly caused by drugs such as penicillins, cephalosporins, bupropion, thiouracil, fluoxetine, and sulfonamides. Other precipitating agents include antilymphocyte globulin, streptokinase, streptococcal infections, and Hep B.
Historically, serum sickness occurred after injection of foreign serum (for example, horse serum), which is why it is called “serum sickness.” It typically presents 7-10 days after exposure to the antigen with fever, chills, arthralgia, urticaria, rash, arthritis, and glomerulonephritis. Immune complexes form throughout the body, fix complement, and activate leukocytes, leading to tissue damage.
Some type III hypersensitivity reactions can occur due to persistent infection (for example, subacute bacterial endocarditis and chronic viral hepatitis) and in autoimmune disorders like SLE. It can also be seen after exposure to high concentrations of inhaled allergens such as mold and hay in farmer’s lung.
Type IV: Type IV hypersensitivity is also called delayed hypersensitivity and is mediated by T cells. A full-blown response takes 24-72 hours to manifest.
| Type | Cells involved | Mechanism |
| Tuberculin or lepromin tests | Th1 cells | Activated T cells release gamma interferon, TNF beta, TNF alpha, GM-CSF , IL3 and chemokines; followed by inflammation |
| Cutaneous or contact hypersensitivity | CD4 or CD8 cells | Protein -hapten complexes sensitize Langerhans cells in the dermis, which then activate T cells. In elicitation phase, repeat exposure causes memory T cells to release cytokines like gamma interferon and IL 17 which stimulate keratinocytes to release cytokines and chemokines, causing local inflammation |