Menopause is the permanent cessation of menstruation due to loss of ovarian function. Over the reproductive years, the number of ovarian follicles steadily declines, and this decline accelerates in the late thirties.
As follicle number falls, inhibin production by granulosa cells gradually decreases. Lower inhibin removes inhibition of FSH, so FSH levels rise. For a few years before menopause, the elevated FSH can increase ovarian estradiol production, which often leads to menstrual irregularities. During this transition:
With progression to menopause, estradiol and inhibin levels decline, while FSH and LH remain elevated. Gonadotropin levels greater than 30 mIU/ml are typically diagnostic of menopause, with an FSH:LH ratio greater than 1.
After menopause, most estrogen comes from peripheral conversion of adrenal androgens. This conversion occurs in the liver, kidney, brain, adrenal, and peripheral adipose tissue. Estrone is the main estrogen produced, and low levels of estradiol are also present due to peripheral conversion of estrone. Obese women have a higher concentration of free estradiol because sex hormone-binding globulin is decreased and aromatization is increased.
Menopause is associated with:
The decline in estrogen also increases the risk of osteoporosis. Vasomotor instability appears to result not from a lack of estrogen, but from estrogen withdrawal. Hot flashes tend to be more severe during stress and more frequent and severe at night (night sweats). Hot flashes are accompanied by pulses of LH and increases in ACTH, cortisol, dehydroepiandrosterone, and androstenedione.
| Unavoidable Risk Factors | Avoidable Risk Factors | Protective Factors |
| Genetic predisposition | Lack of physical exercise | Obesity |
| Low bone mass | Insufficient calcium intake | Multiparity |
| Slender build | Smoking | Muscular habitus |
| White or Asian race | Excessive alcohol intake | Black race |
| Premature ovarian failure | Excessive caffeine intake | Prolonged oral contraceptive use |
| Surgical menopause | Estrogen deficiency | Hormone replacement therapy |
| Glucocorticoid therapy | Anorexia nervosa | |
| Nulliparity | Excessive exercise | |
| Excessive thyroid replacement |
Testosterone is secreted by the Leydig cells of the testes. The testicular enzyme 17 beta hydroxysteroid dehydrogenase converts androstenedione to testosterone. The enzyme 5 alpha reductase converts testosterone to dihydrotestosterone (DHT).
In plasma, testosterone circulates bound to sex hormone-binding globulin and albumin. Only the free (unbound) hormone is biologically active.
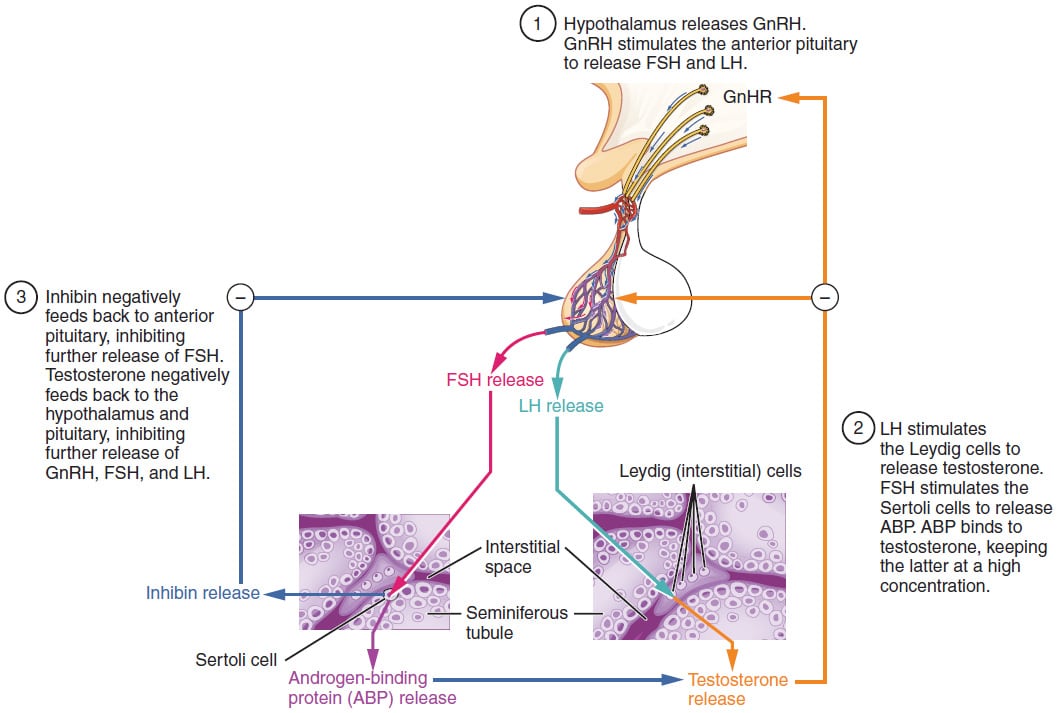
Pulsatile release of GnRH stimulates the anterior pituitary to release FSH and LH:
Testosterone has both paracrine and endocrine effects. It supports Leydig cell function and promotes spermatogenesis. Testosterone also provides negative feedback to:
Sertoli cells secrete:
Sign up for free to take 7 quiz questions on this topic