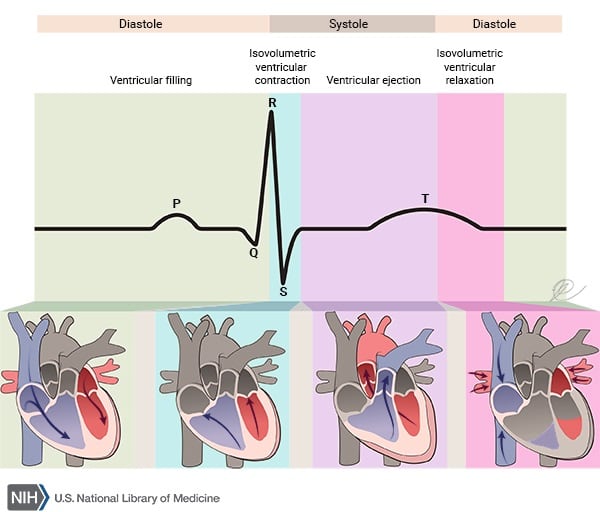
The heart works in a repeating cycle in which systole (contraction) and diastole (relaxation) alternate. The electrical, mechanical, and valvular events that drive this pattern also occur in a coordinated sequence called the cardiac cycle. In each cycle, the heart spends about ⅔ of the time in diastole and ⅓ in systole. There are seven phases of the cardiac cycle:
Atrial contraction against a stiff, less compliant ventricle produces the fourth heart sound (S4). It can be seen in hypertension and in old age. The “a” wave on the JVP is lost in atrial fibrillation (AF). Large “a” waves, called cannon “a” waves, are seen in complete AV block.
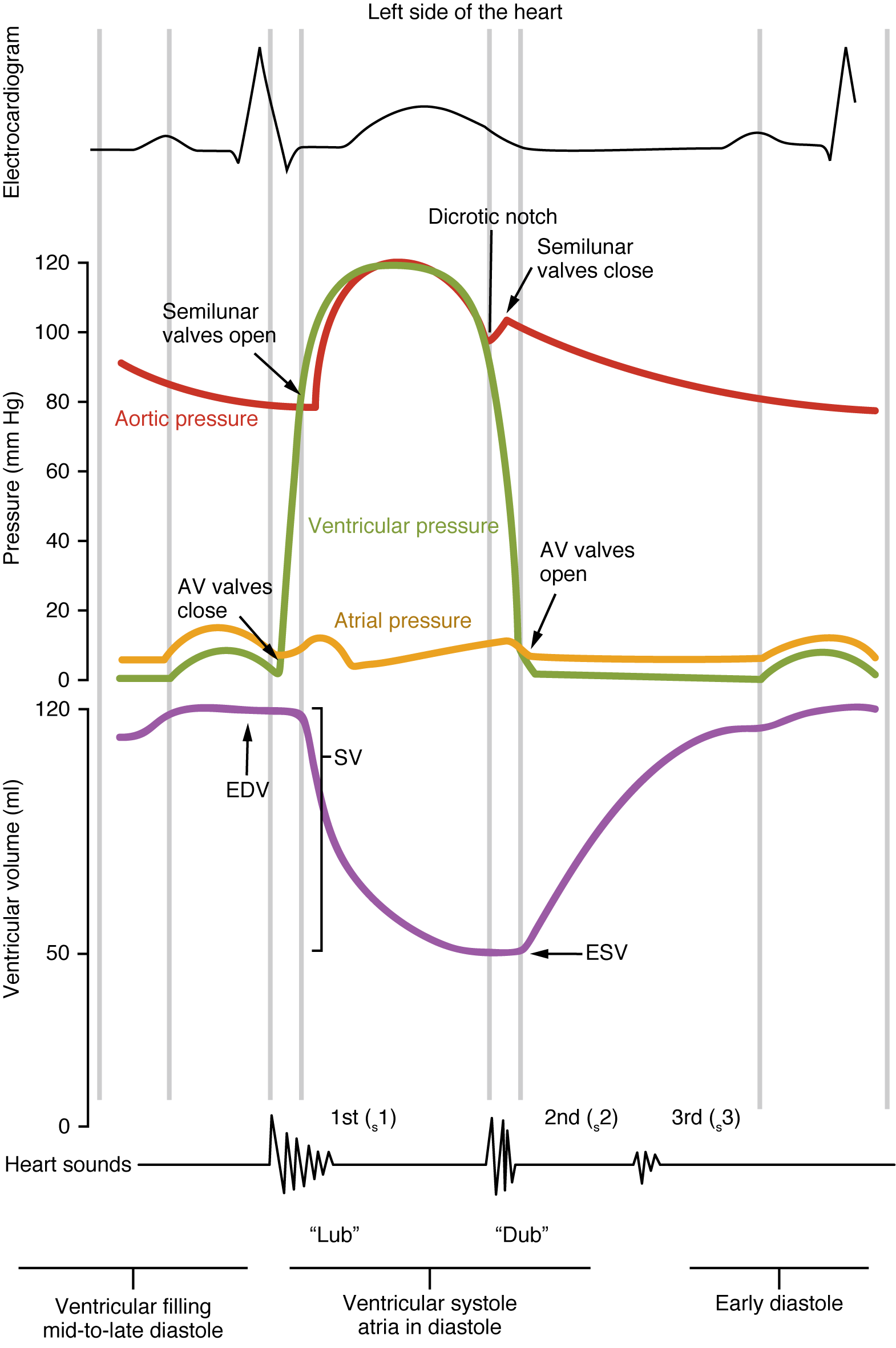
Isovolumetric contraction: The ventricles contract while the AV valves and the semilunar valves (pulmonary and aortic) are closed, so the ventricles act as a closed chamber. The ventricular volume at this point equals the end-diastolic volume (EDV). Because no blood leaves the ventricle during this phase, the volume stays constant, which is why it’s called isovolumetric contraction. This phase corresponds to the QRS complex on the ECG (ventricular depolarization). Ventricular contraction rapidly raises intraventricular pressure. When ventricular pressure exceeds atrial pressure, the AV valves close, producing the first heart sound (S1). Bulging of the mitral valve leaflets into the left atrium produces the positive “c” wave on the JVP, followed immediately by a negative “x” descent.
Rapid ejection: As intraventricular pressure continues to rise and exceeds the pressures in the aorta and pulmonary artery, the aortic and pulmonary valves open. Blood is ejected into the major arteries. Peak ventricular pressures are reached early in the ejection phase.
Reduced ejection: This phase coincides with the T wave on the ECG. Ventricular pressure begins to fall, and the rate of ejection decreases. The AV valves are still open. The volume of blood remaining in the ventricle at the end of this phase is the end-systolic volume (ESV).
Isovolumetric relaxation: All valves (AV, aortic, and pulmonary) are closed again, and the ventricles relax. This marks the beginning of diastole. Because the ventricular volume does not change during this phase, it’s called isovolumetric relaxation, and the ventricular volume remains the ESV. The aortic and pulmonary valves close when ventricular pressure falls below aortic and pulmonary artery pressures, respectively. A dicrotic notch (incisura) appears on the aortic and pulmonary artery pressure tracings due to a brief backflow of blood toward the ventricles as these valves close.
The second heart sound (S2) occurs when the aortic and pulmonary valves close. Because the pulmonary valve normally closes slightly later than the aortic valve, S2 is normally split. This split increases during inspiration because venous return to the right heart increases, delaying P2. During this time, the left atrium fills with oxygenated blood from the pulmonary veins, causing a gradual rise in left atrial pressure recorded as a positive “v” wave. Right atrial filling produces a corresponding “v” wave on right-sided pressure tracings.
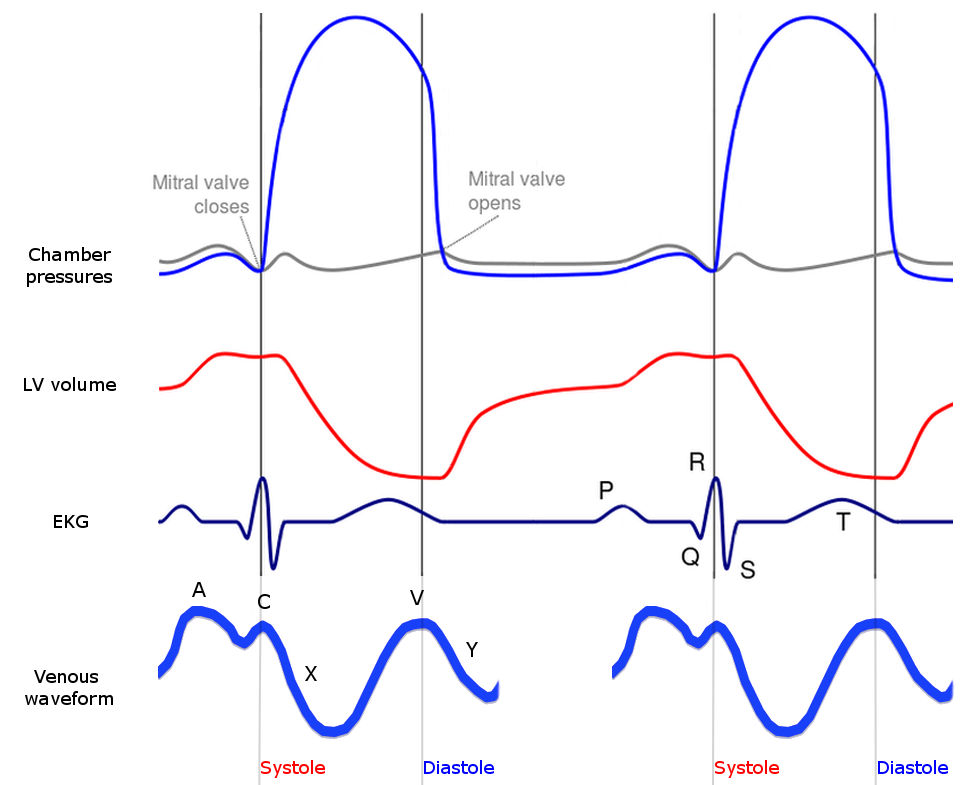
Rapid filling: When ventricular pressure falls below atrial pressure, the AV valves open and blood rapidly flows from the atria into the ventricles. As the atria empty, atrial pressure falls, producing the “y” descent on the JVP (or atrial pressure tracing). If present, the third heart sound (S3) is heard during this phase. S3 is an early diastolic sound, also called a “gallop rhythm.” It can be heard physiologically in children, pregnant women, and young adults, and pathologically due to ventricular dysfunction or volume overload in dilated or hypertrophic cardiomyopathies, acute valve regurgitation, heart failure, anemia, complete AV block, thyrotoxicosis, and left-to-right intracardiac shunts, etc.
Reduced filling or diastasis: The ventricles continue filling from the atria. During this phase, intraventricular pressure steadily rises while atrial pressure falls. Diastasis is the longest phase of the cardiac cycle, and its duration shortens as heart rate increases.
Sign up for free to take 13 quiz questions on this topic