Hyperthyroidism is increased production and secretion of thyroid hormones. Thyrotoxicosis is the clinical syndrome caused by excess circulating thyroid hormones.
i) Diffuse toxic goitre or Grave’s disease or Basedow disease: This is caused by autoantibodies against the TSH receptor. These antibodies stimulate TSH receptors on follicular cells, leading to increased thyroid hormone production. It is more common in women. The thyroid is diffusely enlarged and hypervascular. A bruit may be heard over the thyroid. Histology shows follicular and papillary hyperplasia with stromal lymphocytic infiltration.
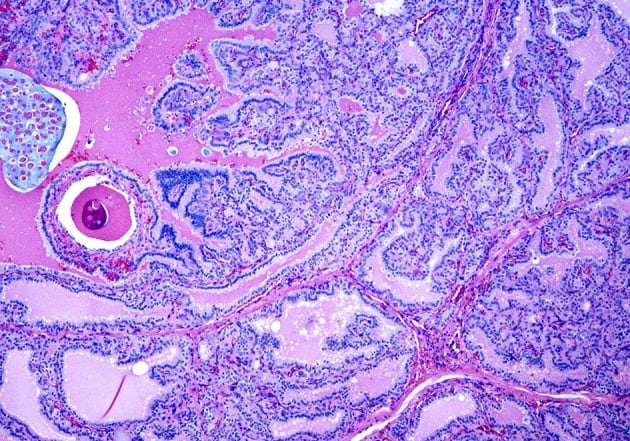
A case of Graves’ disease on medium power showing cells with round nuclei and even chromatin pattern lining the hyperplastic papillae.
ii) Toxic multinodular goitre: In this disorder, the thyroid has multiple nodules with follicular and papillary hyperplasia and lymphocytic infiltration. It occurs in both men and women, typically in older age groups. Atrial fibrillation is commonly associated.
iii) Follicular adenomas/toxic adenoma or Plummer’s disease: Also called hyperplastic nodules, these are benign tumors that secrete excess thyroid hormones. This suppresses hormone production in the rest of the thyroid. They are seen in women.
iv) Struma ovarii: This refers to thyroid tissue within ovarian teratomas (dermoid cysts). Struma ovarii contains > 50% thyroid tissue and can cause hyperthyroidism.
Hyperthyroidism presents with tremors, tachycardia, weight loss despite increased appetite, heat intolerance, and sweating. Other features include proximal myopathy, atrial fibrillation, heart failure, onycholysis (Plummer nails), and brisk tendon reflexes. Grave’s disease has characteristic pretibial myxedema and exophthalmos.
Laboratory diagnosis is based on thyroid hormone assays: TSH, free T4, and total T3. TSH receptor antibodies are present in Grave’s disease.
| Thyroiditis, ectopic thyroid hormone secretion, exogenous thyroid hormone | Low TSH, elevated total, free T4 and total T3, low uptake on radioiodine scan |
| Grave’s disease | Low TSH, elevated free T4 and total T3, homogeneously high uptake on radioiodine scan |
| Toxic multinodular goitre | Low TSH, elevated free T4 and total T3, multiple areas of high uptake on radioiodine scan |
| Toxic adenoma | Low TSH, elevated free T4 and total T3, single area of high uptake with low uptake of rest of the thyroid gland on radioiodine scan |
| TSH secreting pituitary adenoma | Elevated TSH, elevated total and free T4 and total T3 |
| Subclinical hyperthyroidism | Low TSH, normal total T4 and total T3, normal free T4 |
Treatment of beta-adrenergic symptoms (tachycardia, palpitations, tremors) is with beta blockers. Propranolol or atenolol can be used. Propranolol also blocks peripheral conversion of T4 to T3 by inhibiting the enzyme 5’ monodeiodinase.
Antithyroid medications are used for long-term control and include methimazole, propylthiouracil (PTU), and radioactive iodine. Common side effects of methimazole and PTU include skin rashes, pruritus, arthralgia, and gastrointestinal distress. Agranulocytosis can occur with both methimazole and PTU. WBC count and LFTs should be monitored at the beginning of therapy and during treatment.
Both drugs can cause hepatitis. PTU more commonly causes hepatic failure, while methimazole may cause cholestasis. Methimazole is contraindicated in the first trimester of pregnancy, so PTU is preferred. Methimazole can cause aplasia cutis and birth defects in the first trimester. However, methimazole is used in the second and third trimesters because PTU carries a higher risk of hepatotoxicity. ANCA-positive vasculitis may occur.
Grave’s disease needs ablation with radioactive iodine. It is contraindicated in pregnancy and lactation due to radioactivity. Radioactive iodine therapy can also be used in toxic multinodular goitre and toxic adenoma.
Thyroidectomy may be needed in resistant cases. Complications include injury to the recurrent laryngeal nerve (unilateral damage causes hoarseness; bilateral damage causes respiratory distress) and accidental parathyroidectomy.
Patients undergoing thyroidectomy for hyperthyroidism must be pretreated with antithyroid medications, potassium iodide, and beta blockers to prevent thyroid storm. Potassium iodide reduces thyroid gland vascularity and decreases thyroid hormone release.
Sign up for free to take 3 quiz questions on this topic