These fungi form broad, nonseptate hyphae with wide-angle branching. They’re especially associated with infections in patients with diabetes, and they’re known to invade tissues and cause necrosis. They can proliferate within blood vessels.
Rhizopus is implicated more often than Mucor species. Invasion of the nasal sinuses is most common. Typical features include facial pain, blood-stained nasal discharge, and proptosis. They may also cause lung infarctions due to blockage of blood vessels. Black, eschar-like necrotic skin lesions may be seen in burn patients and in patients with diabetes.
Diagnosis is made by microscopy and biopsy showing the typical morphology.
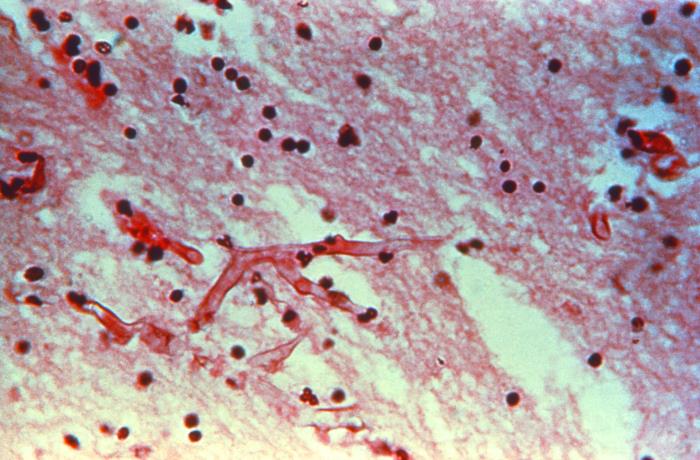
Hematoxylin-eosin ((H&E)-stained specimen, revealed the presence of mycelial fungal filaments in this tissue sample, from a patient ill with mucormycosis (phycomycosis), otherwise known as a form of zygomycosis.
Aspergillosis is a common fungal infection. Aspergillus fumigatus is the most common pathogen in this group. It can cause several distinct clinical syndromes:
Apart from the above, Aspergillus can cause sinusitis, onychomycosis, meningoencephalitis, otomycosis, and endocarditis.
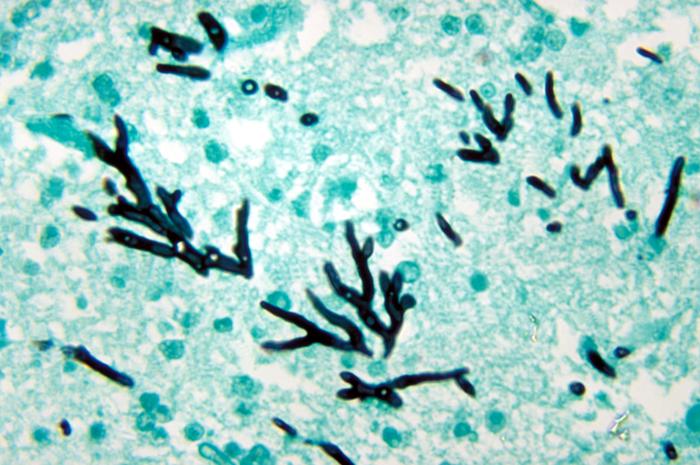
Laboratory diagnosis of Aspergillosis: KOH smears and biopsy samples show characteristic septate hyphae with parallel sides and acute-angle, dichotomous branching. Antibody detection and PCR can be used in some cases. A skin hypersensitivity test will be positive in ABPA.
Pneumocystis jiroveci was previously classified as a protozoan but is now categorized as a fungus. It causes infections in immunocompromised individuals, such as people with HIV, organ transplant recipients, and patients undergoing chemotherapy. Infection is acquired by inhalation. It causes interstitial pneumonia, presenting with fever, cough, dyspnea, and chest pain.
Samples include sputum and bronchoalveolar lavage fluid. A variety of histochemical stains can be used to detect Pneumocystis in clinical specimens, including Diff-Quik, Grocott-Gomori methenamine silver (GMS), and Calcofluor white. GMS is a silver stain, while Calcofluor is a fluorescent method. Immunofluorescence stains that use antibodies directed against P. jiroveci are also available for direct detection in clinical specimens. Samples show numerous cysts, which may appear as crushed ping-pong balls, crescent shapes, folded spheres, flattened beach balls, deflated tennis balls.
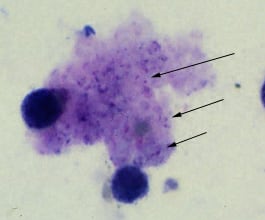
Trophozoites of P. jirovecii in a bronchoalveolar lavage (BAL) specimen from an AIDS patient, stained with Giemsa.
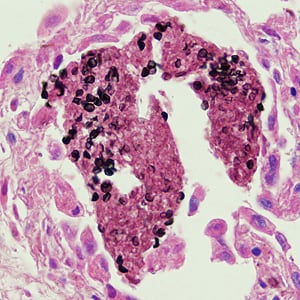
Cysts of P. jirovecii in lung tissue, stained with methenamine silver and hematoxylin and eosin (H&E). The walls of the cysts are stained black; the intracystic bodies are not visible with this stain.
PCR and a blood test to detect beta D Glucan in the cell wall of P. jiroveci can be used for diagnosis. The b2-d-Glucan test is used in the presumptive diagnosis of invasive fungal infections such as Candida spp., Aspergillus spp., and Pneumocystis jirovecii. It is non-invasive, but a drawback is the common occurrence of false-positive results. This test cannot be employed in the diagnosis of Cryptococcosis, Zygomycetes, and Blastomyces dermatitidis.
Sign up for free to take 3 quiz questions on this topic