Obstructive airway or lung disease is characterized by airflow obstruction, seen as decreased expiratory airflow. It primarily involves the bronchi, bronchioles, and/or alveoli. It is seen in asthma, chronic bronchitis, emphysema, COPD, bronchiectasis, alpha 1 antitrypsin deficiency, and bronchiolitis obliterans.
I) Reactive airway disease and asthma: Reactive airway disease is a poorly defined term that’s often used synonymously with asthma. However, “reactive airway disease” does not mean the patient necessarily has asthma. In doubtful cases, pulmonary function tests and a methacholine challenge test can confirm whether a patient has asthma.
“Reactive airway dysfunction syndrome” is the development of an asthma-like syndrome with acute wheezing (most often with no past history of asthma) resulting from a single exposure to an extreme irritant (e.g., fumes, dust storms). Methacholine sensitivity of the airways is seen in reactive airway dysfunction syndrome.
Asthma: Asthma is characterized by chronic airway inflammation and airway hyperresponsiveness, with marked airway narrowing after exposure to triggers such as viruses, dust, pollen, mould, cold air, and exercise. It presents with episodes of wheezing, chest tightness, dyspnea, and coughing that occur in response to one of these triggers. Reversible bronchoconstriction is seen.
Asthma is caused by a Th2 immune response and cytokines IL4, 5, 9, and 13, along with eosinophilic infiltration and release of IgE and mediators such as histamine that drive the pathological processes. An early and late response is seen, leading to progressive inflammation and airway damage. Airway remodelling occurs with frequent asthma exacerbations.
Maternal smoking, delivery by C-section, and the use of antibiotics in pregnancy increase the risk of asthma in offspring. Asthma is often associated with atopy, allergic rhinitis, and eczema. RSV infections in infancy may predispose to asthma in adolescence.
*Normal value of FEV1 in adults is >80% and in children is >90%
**PEF is peak expiratory flow
Challenge tests such as the methacholine challenge are done in adults when clinical suspicion of asthma is high but spirometry is normal. Peak expiratory flow can be measured practically anywhere using a peak flow meter. Peak expiratory flow rate (PEFR) correlates with cross-sectional area, even though the actual site of obstruction in asthma is in the bronchi and bronchioles.
The normal range of PEFR for men is 500-700 L/min, and for women is 380-550 L/min. Asthma exacerbations can be graded as:
Class: Intermittent
Class: Mild persistent
Class: Moderate persistent
Class: Severe persistent
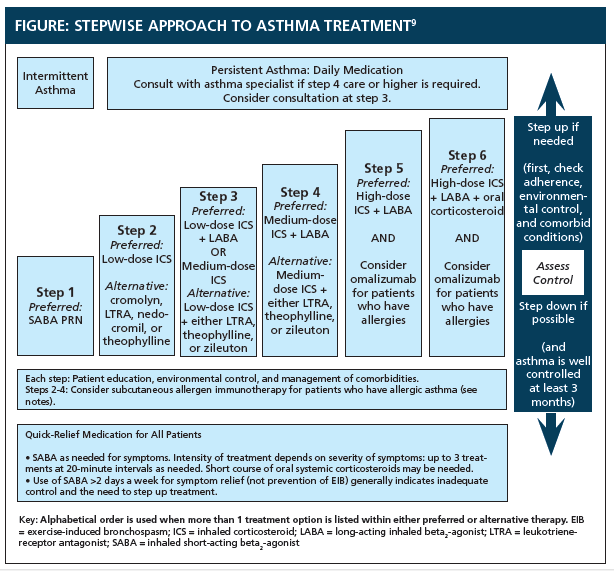
Step-up therapy involves initiating treatment at a low dose and increasing the dose or adding drugs if needed. Step-down therapy starts with a higher-dose regimen, which is then reduced to the minimum needed to maintain adequate symptom control.
Once control of asthma is maintained for 3 months, a gradual reduction of maintenance therapy can be tried to keep therapy at a minimum.
Sign up for free to take 6 quiz questions on this topic