COPD, chronic bronchitis and emphysema:
WHO defines chronic obstructive pulmonary disease (COPD) as a lung disease characterized by chronic obstruction of lung airflow that interferes with normal breathing and is not fully reversible. Diagnosis is made using spirometry along with clinical features such as dyspnea, chronic cough (with or without sputum production), wheezing, etc. Emphysema and chronic bronchitis are the two most common conditions that contribute to COPD.
Smoking is the most common cause of COPD. COPD typically follows a long course with intermittent exacerbations, often triggered by factors such as non-compliance with treatment and infections.
Chronic bronchitis is defined as cough with expectoration for 3 months of the year for at least 2 years. It is more common in men than women. Smoking and pollution are the most common causes.
Smoking impairs ciliary movement and causes hyperplasia and hypertrophy of the mucus glands, which predisposes to chronic bronchitis. The Reid index is increased. It is calculated as the ratio of the thickness of submucosal glands to the total thickness of the bronchial wall. The normal index is <0.4. Squamous metaplasia and dysplasia may be present.
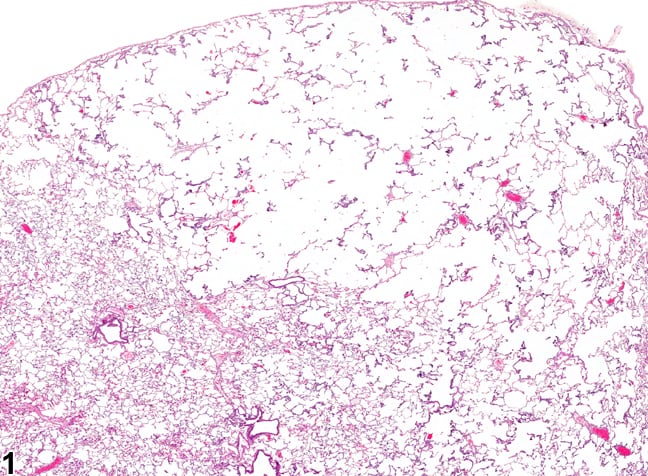
Emphysema is permanent dilation of air spaces distal to the terminal bronchioles along with destruction of alveolar walls. Chronic bronchitis and emphysema often co-exist in the same lung.
Alpha 1 antitrypsin (AAT) deficiency causes emphysema and is inherited in an autosomal codominant pattern. Antitrypsin is a type of serine protease inhibitor (serpin). Alpha-1 antitrypsin is produced in the liver and transported to the lungs via the blood. It protects the lungs from neutrophil elastase, which can damage lung tissue if not properly controlled. Without enough functional alpha-1 antitrypsin, neutrophil elastase destroys alveoli and causes emphysema.
The SERPINA1 gene normally codes for alpha 1 antitrypsin. M, Z, and S are some of the alleles of the SERPINA1 gene. Normal individuals have the MM pattern and therefore no deficiency. The ZZ pattern leads to severe deficiency of AAT. The S allele is associated with moderate risk.
The frequency of AAT deficiency is higher in individuals with European ancestry. Environmental factors such as exposure to tobacco smoke, chemicals, and dust likely affect the severity of alpha-1 antitrypsin deficiency.
In addition to emphysema, AAT deficiency is associated with cirrhosis, increased risk of hepatocellular carcinoma, and panniculitis. Diagnosis is made by estimating levels of AAT in blood and is confirmed by genetic testing. Serum protein electrophoresis will show an absent or decreased alpha-1 band (AAT is an alpha globulin). Gross examination of lung sections will show multiple dilated air spaces.
Sign up for free to take 4 quiz questions on this topic