Mechanics of breathing:
Muscles of respiration: The diaphragm is the most important muscle for respiration. When it contracts, intrathoracic volume increases and intrathoracic pressure decreases, which draws air into the lungs (inspiration).
External intercostal muscles and accessory muscles (e.g., scalenes, pectorals) become important when the respiratory rate and the effort of breathing increase, such as during respiratory distress.
When extra effort is needed for exhalation, the abdominal muscles (rectus abdominis, internal and external obliques) along with the internal intercostals are recruited.
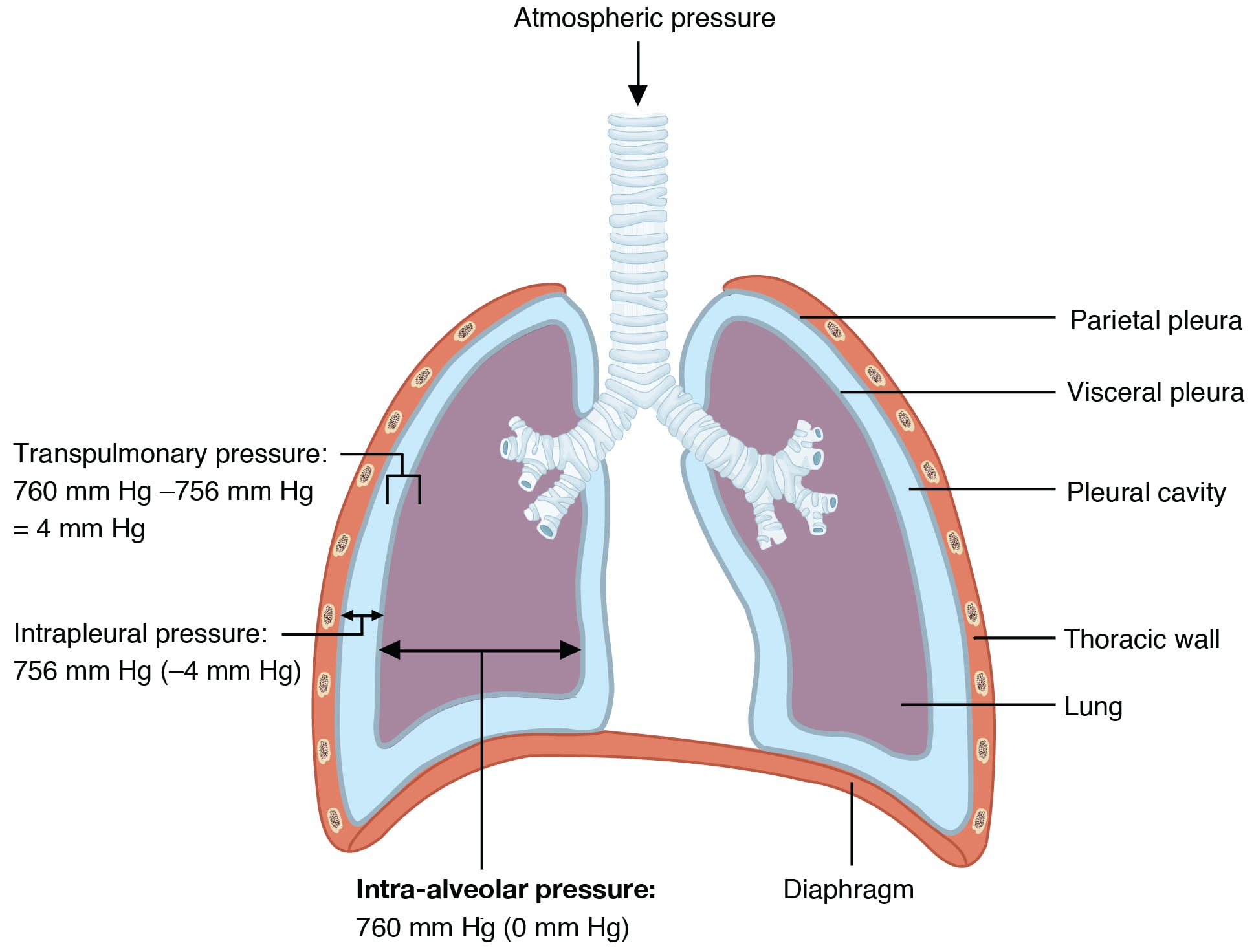
Transpulmonary pressure: As the lungs fill with air, the pressure inside the alveoli becomes more positive, while the pressure outside the alveoli (in the pleural space) remains negative. This negative outside pressure distends the alveoli and helps them fill with air. If the outside pressure becomes positive, the alveoli can collapse.
Ptp = Palv - Pip. (where Ptp is transpulmonary pressure, Palv is alveolar pressure, and Pip is intrapleural pressure)
Under physiological conditions, transpulmonary pressure is always positive. Intrapleural pressure is always relatively negative and large, while alveolar pressure moves from slightly negative to slightly positive as a person breathes.
The lung has an inherent tendency to recoil inward due to its elasticity, while the chest wall tends to recoil outward. These opposing forces create a relatively negative intrapleural pressure. This negative intrapleural pressure helps keep small airways (which lack cartilaginous support) patent.
During inspiration, Pip becomes more negative, which makes Palv lower than atmospheric pressure, so air flows into the alveoli. Expiration is usually a passive process, aided by elastic recoil of the lung.
"Intrapulmonary and Intrapleural Pressure Relationships: Alveolar pressure changes during the different phases of the cycle. It equalizes at 760 mm Hg but does not remain at 760 mm Hg. "
Compliance of the lung: Lung compliance is the change in lung volume per change in transpulmonary pressure (Ptp). When Ptp is zero, the lung can neither inflate nor deflate.
At functional respiratory capacity (FRC), Palv equals atmospheric pressure. At FRC, the inward recoil tendency of the lungs equals the outward recoil tendency of the chest wall.
Compliance is lowest at the extremes of FRC. This means that both a very expanded lung and a completely deflated lung have a lower ability to distend for a given pressure change.
Compliance can be estimated by the slope of the pressure-volume loop of the lung. A steeper slope (increased slope) corresponds to increased compliance, and a flatter slope corresponds to decreased compliance.
The work of breathing: The work of breathing is usually estimated by the area under the dynamic pressure-volume curve of the lungs. Under physiological conditions, the work needed for inspiration is greater than that needed for expiration.
Restrictive lung diseases (e.g., interstitial lung diseases, pneumonia, surfactant deficiency such as acute respiratory distress syndrome, hemothorax, pneumothorax, empyema, pleural effusion or thickening, respiratory muscle weakness, chest deformities, cardiomegaly) are associated with decreased compliance of the lungs, the chest wall, or both. This results in a rightward shift of the static and dynamic pressure-volume loop of the lungs, chest wall, or both. FRC will be lower.
In obstructive lung diseases (e.g., bronchial asthma, emphysema, chronic bronchitis, bronchiectasis), pulmonary compliance is normal or increased, especially if emphysematous lung changes co-exist. Dynamic lung compliance curves are either not displaced or shifted leftward if emphysematous lung changes develop. FRC will be higher. The main defect is increased airway resistance, especially during expiration.
Surfactant: Surfactant is synthesized by type II alveolar epithelial cells. Its primary component is a phospholipid called dipalmitoyl phosphatidylcholine (DPPC), which reduces surface tension in the alveoli. Without surfactant, small alveoli collapse because they have a higher collapsing pressure.
Surfactant reduces alveolar collapsing pressure, increases compliance, and reduces the work of breathing. Glucocorticoids increase surfactant production. In intrauterine life, surfactant is produced after 24 weeks of age. Premature infants are predisposed to respiratory distress syndrome due to insufficient surfactant. Pulmonary edema, pulmonary hemorrhage, and meconium aspiration can inactivate surfactant and cause respiratory distress.
Airway resistance: Airway resistance is inversely proportional to the fourth power of the radius. The medium-sized airways (not the small airways) are the site of greatest resistance. This is because, although small airways have a smaller diameter, they are arranged in parallel, which decreases total resistance. Parasympathetic stimulation increases airway resistance, while sympathetic stimulation decreases airway resistance.
Ventilation and perfusion of the lung (V/Q): Perfusion of the lung depends on three factors: alveolar pressure (Palv), pulmonary arterial pressure (Pa), and pulmonary venous pressure (Pv). Higher Palv can compromise blood flow in the local pulmonary circulation because pulmonary vessels are thin-walled and under lower pressure.
Based on the influence of gravity, perfusion of the lung is divided into three zones from superior to inferior: I, II, and III.
In zone I (apex), Palv > Pa > Pv. Arterial blood flow is very low, which adds to physiological dead space. Zone I is not normally seen in healthy individuals, but it can occur with positive pressure ventilation, hemorrhage, etc., and it adds to dead space.
In the middle zone (zone II), Pa > Palv > Pv.
In the lower zone (zone III), Pa > Pv > Palv, and perfusion is highest.
During exercise, Pa increases, eliminating any existing zone I.
Ventilation and perfusion both increase from top to bottom in the lung, but perfusion increases more than ventilation. The average V/Q ratio for the lung is 0.8. The V/Q ratio is highest at the apex and lowest at the base of the lung. In zone I (highest V/Q), PaO2 is highest and PaCO2 is lowest, while in zone III, PaO2 is lowest and PaCO2 is highest.
A mismatch of ventilation and perfusion is called a V/Q defect. When perfusion stops (e.g., pulmonary embolism), V/Q becomes infinity and dead space increases. When ventilation is obstructed, V/Q becomes 0 and blood is shunted away from non-ventilated regions to ventilated regions of the lung. Depending on the severity of the ventilation and/or perfusion defect, the V/Q ratio will change.
Sign up for free to take 10 quiz questions on this topic