Special senses
Vision
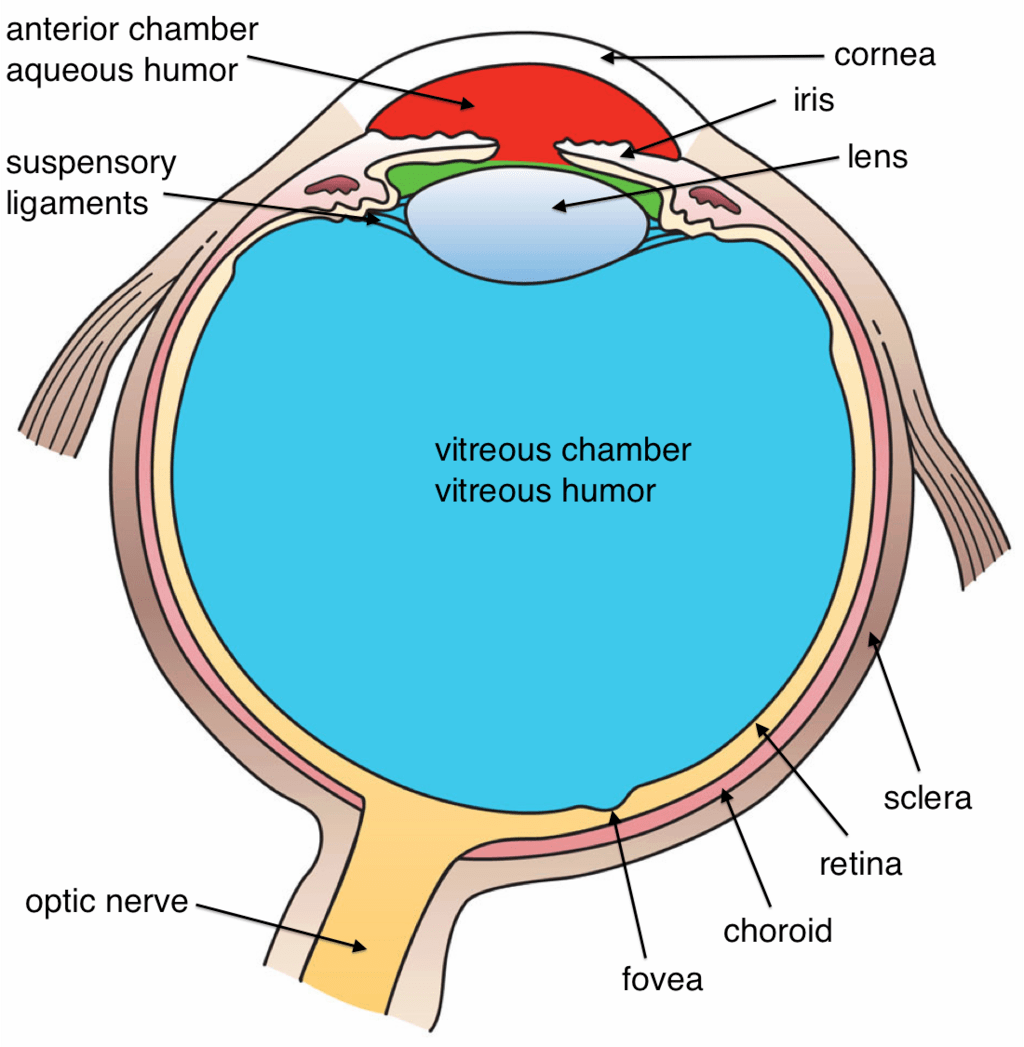
The eye has three main layers:
- Outer layer: thick, fibrous sclera (white of the eye), conjunctiva, and the clear cornea
- Middle layer (uvea): pigmented, vascular layer made of the iris, ciliary body, and choroid
- Inner layer: the retina
The cornea lies anterior to the iris, ciliary body, and lens.
The eye also has three chambers:
- Anterior chamber: between the cornea and iris
- Posterior chamber: between the iris and lens
- Vitreous chamber: between the lens and retina
The anterior and posterior chambers are filled with clear aqueous humor, while the vitreous chamber is filled with gelatinous vitreous humor.
Aqueous humor is continually produced by the ciliary body. It flows through the posterior and anterior chambers to nourish the cornea and lens. It then drains through the trabecular meshwork into the canal of Schlemm and finally into the systemic circulation.
Light enters the eye through the transparent cornea and lens. It is refracted and focused onto the retina, where it stimulates photoreceptors (rods and cones). This ultimately generates action potentials in the optic nerve. The optic nerve and visual pathway carry this information to the cerebral cortex, allowing you to see and to perceive color and movement.
The iris contains two key muscles that control pupil size (and therefore how much light enters the eye):
- Sphincter pupillae: parasympathetic control from the Edinger-Westphal nucleus of the oculomotor nerve, relayed through the ciliary ganglion
- Dilator pupillae: sympathetic control, innervated from the T1 spinal segment through the superior cervical ganglion
The lens is suspended by suspensory ligaments attached to the ciliary body, which contains the ciliary muscle. When the ciliary muscle contracts, the suspensory ligaments become lax, allowing the lens to increase its curvature (as in accommodation). This is under parasympathetic control and is innervated by the oculomotor nerve.
The rods and cones are the photoreceptors of the eye. Each has:
- an outer segment for signal transduction
- an inner segment containing cell organelles
Rods outnumber cones.
- Rods: high light sensitivity but low spatial resolution; responsible for scotopic (night) vision
- Cones: less light sensitive; responsible for photopic (daytime) vision, color vision, and visual acuity
Cone types:
- L cones respond to red wavelengths
- M cones respond to green wavelengths
- S cones respond to blue wavelengths
In moonlight or starlight, both rods and cones are stimulated; this is called mesopic vision.
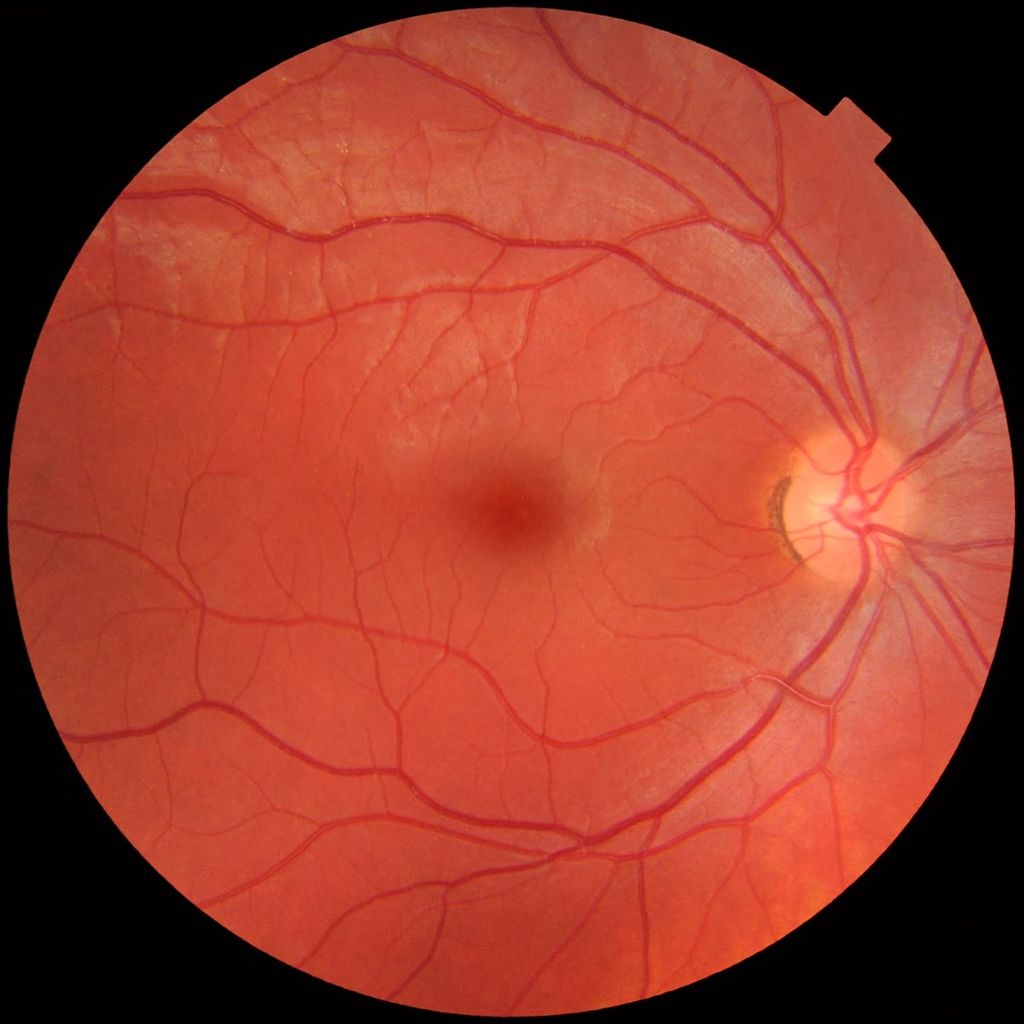
On fundoscopy, the optic nerve appears as a circular to oval white area in the center of the retina. This is the optic disc (optic nerve head). Blood vessels radiate outward from the optic disc. Because rods and cones are absent at the optic disc, it forms the blind spot.
A little to the left of the optic nerve, you can see an oval, reddish area without blood vessels called the fovea. A depression in its center is the foveal pit, which contains only densely packed cones, making it the area of highest visual acuity.
The yellow-tinged, circular macula lutea surrounds the fovea. Carotenoid pigments such as lutein give the macula its yellow color and protect the delicate fovea from harmful ultraviolet radiation.
- The retina around the fovea is the central retina (higher number of cones).
- The retina farther away is the peripheral retina (more rods).
Clinical correlations:
- In retinitis pigmentosa, rods degenerate first, causing tunnel vision.
- In macular degeneration, the retinal pigment epithelium degenerates, forming drusen and affecting the macula and fovea. This leads to cone death and a detrimental impact on visual acuity.
Fundus photograph showing the blood vessels in a normal human retina. Veins are darker and slightly wider than corresponding arteries. The optic disc is at right, and the macula lutea is near the centre.
The retina is a multilayered structure made of pigment cell, photoreceptor, outer nuclear, outer plexiform, inner nuclear, inner plexiform, ganglion cell and optic nerve layers. Axons of the retinal ganglion cells form the optic nerve.
The outer segments of photoreceptors contain photopigments, which are made of 11 cis-retinal (derived from vitamin A) bound to an opsin protein:
- Rhodopsin in rods
- Iodopsin in cones
When photons of light strike the outer membrane, they cause photoisomerisation of 11-cis retinal to all-trans retinal. This activates a G protein called transducin, which activates a phosphodiesterase that converts cGMP to 5’ GMP. As cGMP levels fall, Na channels close, blocking inward sodium flux and causing hyperpolarization of the cell membrane.
In the dark, the opposite occurs: cGMP increases, Na channels open, and the photoreceptor depolarizes. These membrane potential changes influence the secretion of excitatory and inhibitory neurotransmitters.
Neuronal connections in the retina:
- Rods and cones synapse with bipolar cells, which are the first order neurons in the visual pathway.
- ON bipolar cells depolarize in response to light.
- OFF bipolar cells hyperpolarize in response to light.
- Bipolar cells synapse with ganglion cells, which form the second order neurons in the visual pathway.
- P type ganglion cells (midget cells): specialized for color vision and spatial resolution
- M type ganglion cells (parasol cells): specialized for movement detection
Ganglion cell axons converge at the optic disc to form the optic nerve. The optic nerve is developmentally and functionally part of the CNS, and its sheath is laid down by oligodendrocytes.
A special type of retinal ganglion cell expressing melanopsin is photosensitive but does not contribute to image-processing or vision; it is involved in circadian rhythms.
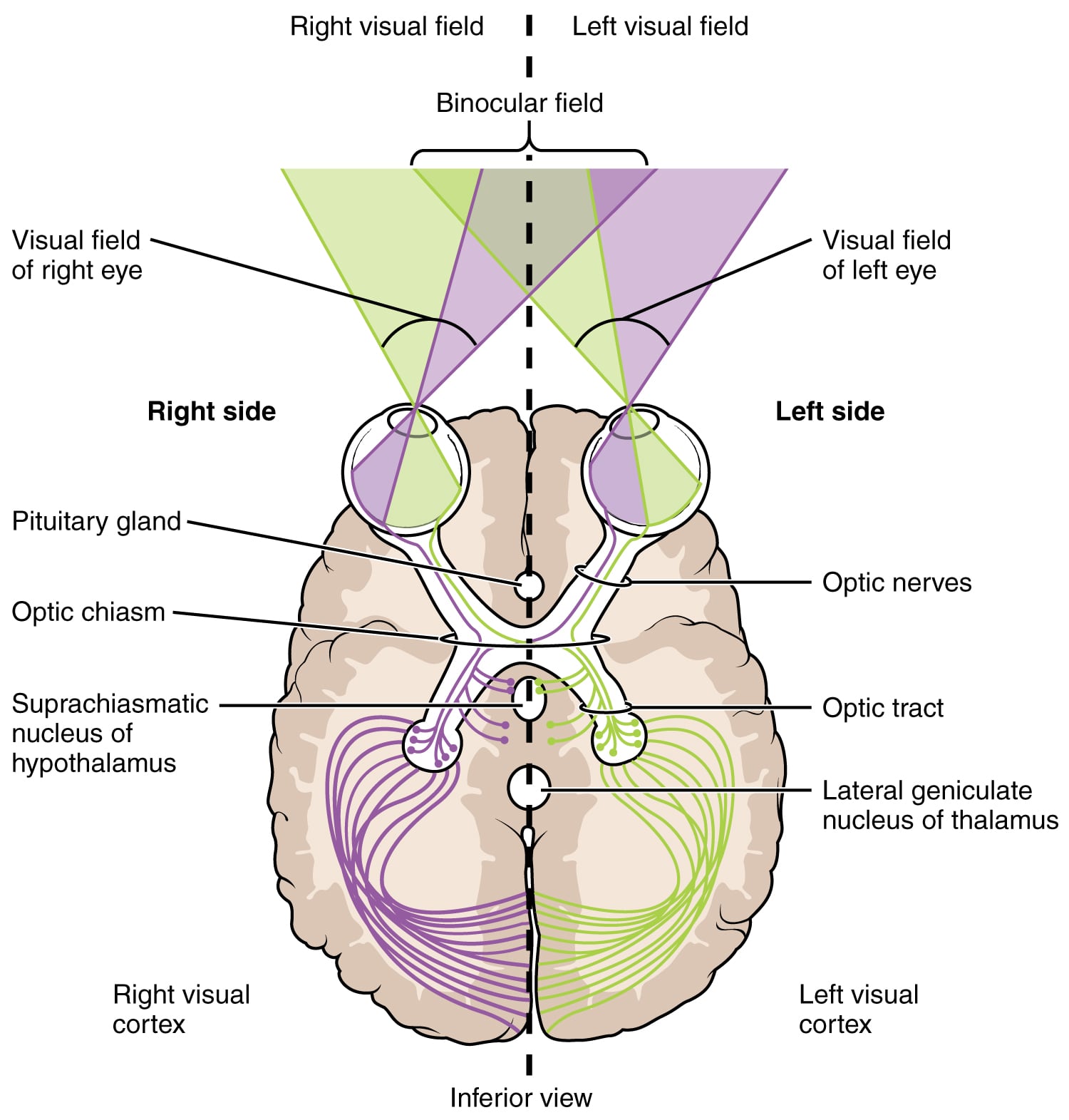
The retina is tentatively divided into a medial (nasal) half and a lateral (temporal) half:
- The nasal retina receives visual input from the temporal visual field.
- The temporal retina receives visual input from the nasal visual field.
Each optic nerve carries input from both the nasal and temporal retina of that eye. The optic nerves meet above the pituitary gland to form the optic chiasma, where some fibers cross.
- Fibers from each nasal retina (carrying input from the temporal visual field) cross to the opposite side at the optic chiasma.
This crossing forms the optic tracts.
The optic tract on each side terminates in the corresponding lateral geniculate nucleus (LGN) of the thalamus, which is the third order neuron of the visual pathway. The visual radiation arises from the LGN and projects to the primary visual cortex (Brodmann area 17) in the occipital lobe.
Anatomy around the calcarine sulcus:
- The cuneus gyrus is located superior to the calcarine sulcus and receives lower quadrants of the visual hemifields.
- The lingual gyrus is located inferior to the calcarine sulcus and receives superior quadrants of the visual hemifields.
The inferior part of the visual radiation forms Meyer’s loop, which travels through the temporal lobe before terminating in the lingual gyrus.
In the primary visual cortex, the peripheral retina is represented inwards, and the central retina (including the fovea and macula) is represented outwards.
| Site of lesion | Visual field defect | Comments |
| Right optic nerve | Right eye blindness | |
| Optic chiasma | Bitemporal heteronymous hemianopsia* | Craniopharyngioma, pituitary adenoma, aneurysm of ACA and anterior communicating artery** |
| Right Optic tract | Left homonymous hemianopia | Occlusion of anterior choroidal artery |
| Right Optic radiation (entire) | Left homonymous hemianopia | Occlusion of the thalamogeniculate branch of the PCA. |
| Right Meyer’s loop | Left homonymous superior quadrantanopia | Stroke of Inferior division of MCA |
| Right non-Meyer’s loop (superior part) of optic radiation | Left homonymous inferior quadrantanopia | PCA stroke |
| Right Primary visual cortex | Left homonymous hemianopia with macular sparing | PCA stroke*** |
| Retina | Scotomas | Small spots of deficits |
*Heteronymous means both right and left. Homonymous means only right or only left.
** Initially these lesions may manifest as quadrantanopia i.e. only a quadrant of the visual field will be involved before involving the hemifield.
*** The Macular cortex has dual blood supply from PCA and MCA.
Pupillary light reflex: When light is directed at one eye, the pupil of that eye constricts due to the direct light reflex. At the same time, the pupil of the opposite eye constricts due to the consensual (indirect) light reflex.
- The sensory (afferent) limb of the light reflex is the optic nerve.
- Fibers involved in the light reflex travel to the pretectal nuclei, which project bilaterally to both Edinger-Westphal nuclei in the midbrain.
- The Edinger-Westphal nucleus is the parasympathetic nucleus of the oculomotor (III) cranial nerve.
- The Edinger-Westphal nuclei innervate the parasympathetic ciliary ganglion through the oculomotor nerve.
- Postganglionic parasympathetic fibers from the ciliary ganglion travel in the short ciliary nerves to innervate the constrictor pupillae muscle, producing pupillary constriction.
Accommodation reflex: When you focus on a near object, three things happen simultaneously:
- both eyes converge
- the lens becomes more convex
- the pupil constricts
The afferent limb consists of the optic nerve. The motor nucleus of the oculomotor nerve and the Edinger-Westphal nucleus then innervate the medial rectus muscle and sphincter pupillae plus ciliary muscle respectively, causing them to contract. Efferents are carried in the oculomotor nerve.