Fanconi syndrome: This can be congenital or acquired and causes decreased reabsorption in the proximal convoluted tubule. As a result, amino acids, glucose, bicarbonate, phosphate, and uric acid are lost in the urine. Loss of bicarbonate can cause type II renal tubular acidosis. It is seen in cystinosis, tyrosinemia, Wilson disease, galactosemia, fructose intolerance, lead poisoning, Legionella pneumonia, multiple myeloma, ALL, and with medications such as antivirals (e.g., NRTIs), ranitidine, cisplatin, azathioprine, gentamicin, etc. It presents with symptoms of the underlying disorder and may also cause osteomalacia, rickets, dehydration, electrolyte imbalances, metabolic acidosis, failure to thrive, paresthesias, muscle weakness, CCF, etc. Management includes treating the underlying disorder, replacing fluids and electrolytes, vitamin D and phosphate replacement, and correcting acid-base balance.
Vesicoureteral reflux or VUR: This is retrograde flow of urine from the bladder back into the ureters due to improper function of the vesicoureteric junction. As a result, urine backflows into the ureters and sometimes the kidneys during micturition. It commonly presents in childhood. It may be asymptomatic or present with recurrent UTIs, urinary incontinence, bedwetting, constipation, and urinary retention. Recurrent UTIs can cause renal scarring that may progress to ESRD. It may also predispose to HT later in life, especially when UTIs are not diagnosed and treated promptly.
VUR can be primary (more common) or secondary.
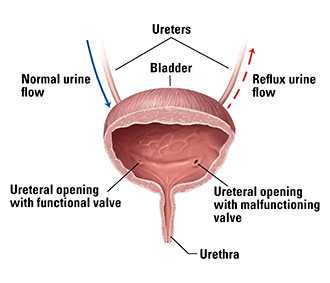
Diagnosis is made with a voiding cystourethrogram (VCUG), which demonstrates reflux. Abdominal ultrasound may show dilated ureters and kidneys. Some cases can be detected on prenatal ultrasound. Management includes treating UTIs, using low-dose prophylactic antibiotics to prevent UTIs, treating the underlying disorder in secondary VUR, intermittent bladder catheterization, and surgery to relieve any stenosis.
Posterior urethral valves: This is a common cause of obstructive uropathy, especially in male infants. Posterior urethral valves cause congenital obstruction of the posterior urethra. The valves may result from incomplete dissolution of the urogenital membrane, hypertrophied urethral folds, or folds of the verumontanum. It may be associated with hypospadias, prune belly syndrome, PUJ obstruction, and renal ectopia.
It may present antenatally with hydronephrosis detected on routine antenatal ultrasound. Other symptoms include poor urinary stream, UTIs, VUR, bedwetting, hematuria, urinary retention, and failure to thrive. ESRD may occur.
Ultrasound may show hydronephrosis, thickened bladder wall, renal cysts, and a keyhole sign in the bladder neck. The investigation of choice is VCUG, which shows a dilated posterior urethra, a trabeculated bladder, VUR, and abnormal valves.
Management includes relieving hydronephrosis and urinary retention with catheter drainage, antibiotics as needed, and monitoring renal function. Definitive treatment includes endoscopic ablation of the abnormal valves. Vesicostomy and upper urinary tract diversion surgery may be needed in resistant cases. Some centers consider antenatal interventions to preserve long-term renal function (if expertise is available), since the disorder begins in early fetal life.
Urethral stricture: This is narrowing of the urethra due to scarring and fibrosis. It is much more common in men than in women. Causes include gonorrhea, balanitis xerotica obliterans, traumatic rupture of the urethra in pelvic fractures, and invasive urethral procedures such as transurethral resection of the prostate, indwelling catheters, brachytherapy, etc. Strictures are most common in the bulbar urethra, while the prostatic and membranous urethra are more commonly involved following pelvic fractures.
Symptoms include straining during urination, incomplete bladder emptying, increased frequency, and urgency. Some patients may present with acute urinary retention. Diagnosis can be confirmed by uroflowmetry, retrograde cystourethrography, and VCUG.
In patients presenting with urinary retention due to urethral stricture, suprapubic (rather than transurethral) catheterization should be performed. Surgical management includes internal urethrotomy, resection of the stricture with end-to-end anastomosis, urethroplasty, and urethrostomy.
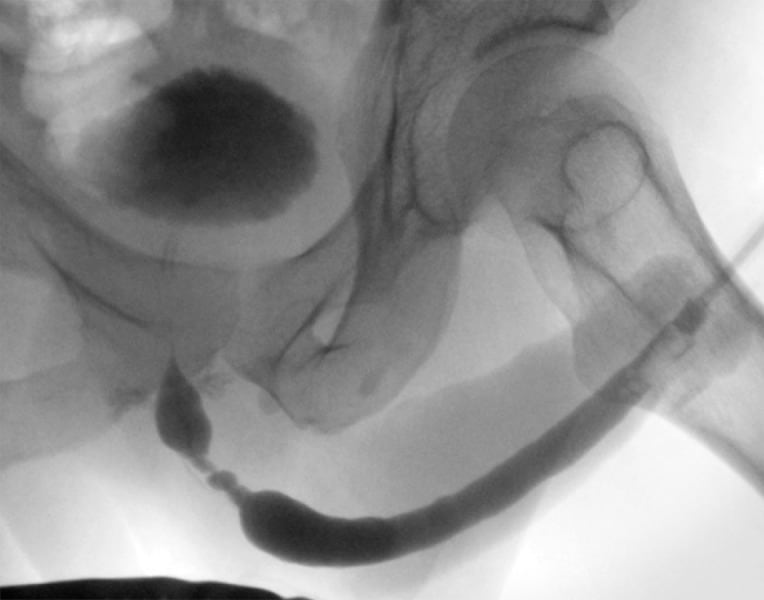
Cystourethrogram of a bulbar urethral stricture about 3 cm in length
Traumatic injuries of the urethra: Injuries of the anterior urethra are most often caused by blunt or penetrating trauma, straddle injuries, and iatrogenic injury from instrumentation. Injuries to the posterior urethra occur with pelvic fractures, such as those seen in traffic accidents.
Signs suggesting urethral injury include blood at the urethral meatus, penile hematoma, and a high-riding prostate. If blood is present at the urethral meatus, avoid urethral instrumentation and catheterization to prevent further urethral damage. Use suprapubic catheterization instead.
The gold standard for diagnosis is retrograde urethrography. In urethral disruption, contrast extravasation into the pelvis is seen. Conservative management is preferred for stretch injuries or partial disruptions, while urethroplasty is performed for complete disruptions.
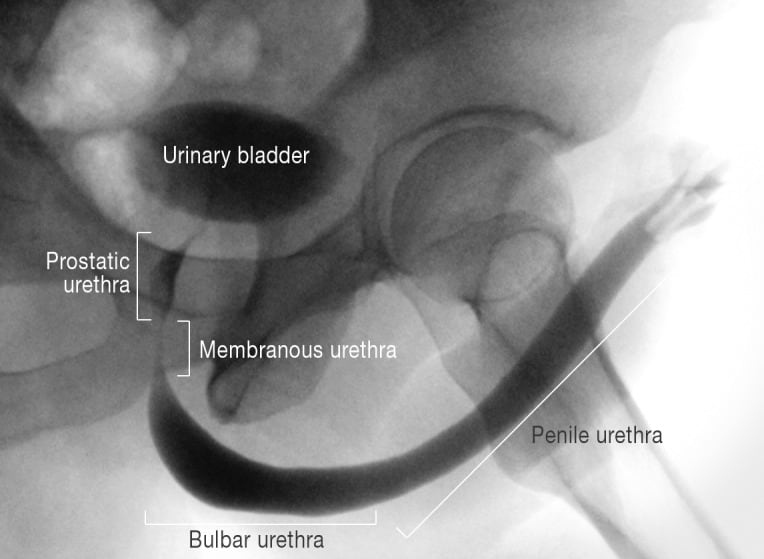
Cystourethrogram of a normal urethra, showing the anatomical segments
Sign up for free to take 2 quiz questions on this topic