Antibiotics may be bactericidal or bacteriostatic.
These drugs kill bacteria. They’re used in situations where you need rapid bacterial clearance, such as:
These drugs inhibit bacterial growth without directly killing the organism. Because the bacteria aren’t killed, they can resume growth once the antibiotic is removed.
With bacteriostatic drugs, you rely on the host immune system to clear the infection. For that reason, bacteriostatic drugs are ineffective in an immunocompromised host.
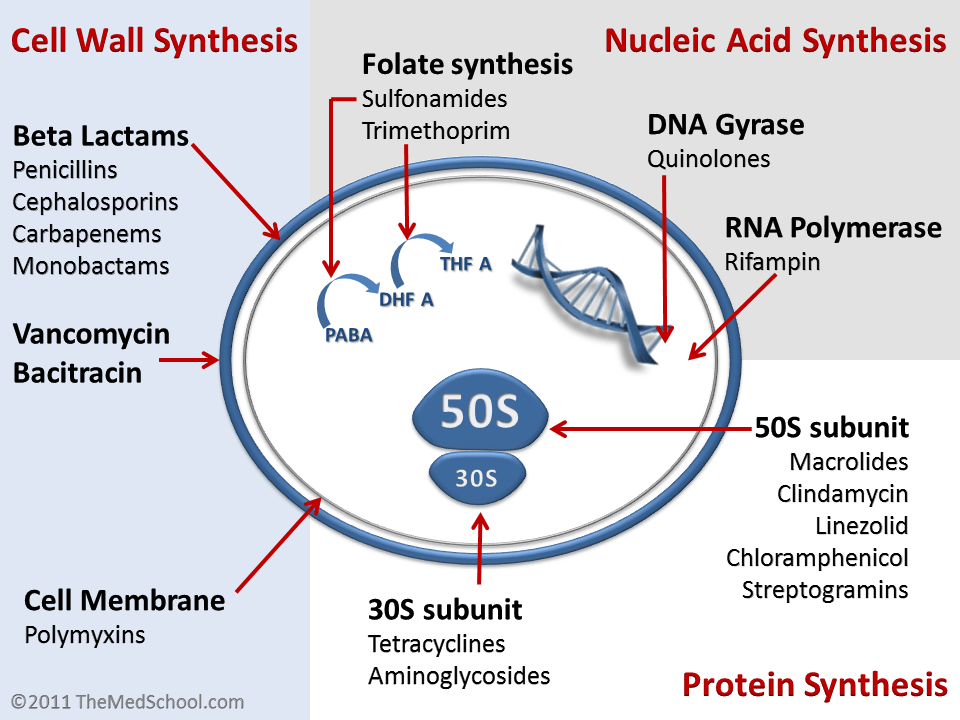
This group includes Beta Lactam antibiotics, Vancomycin, Cycloserine, and Bacitracin.
Penicillin is effective only against actively growing bacteria, so it works best when bacteria are in the log phase of growth.
Penicillins contain a beta lactam ring that mimics the D-alanine D-alanine portion of peptide chains in the bacterial cell wall. Normally, this D-alanine D-alanine sequence is bound by Penicillin Binding Proteins (PBPs). When a PBP binds the beta lactam ring instead, it can no longer participate in peptidoglycan synthesis.
Some PBPs are transpeptidases, which cross-link peptidoglycans in the cell wall. Penicillin inhibits these transpeptidases. In addition, enzymes called murein hydrolases are activated in penicillin-treated cells; these enzymes degrade peptidoglycan and lead to cell lysis.
Although penicillins are bactericidal against gram positive cocci, gram positive bacilli, Neisseria, Treponema pallidum, and anaerobes (except Bacteroides fragilis), they are less effective against gram negative bacilli. This is because they penetrate the outer membrane of gram negative microbes poorly.
Some exceptions are modified penicillins:
Their mechanism of action is very similar to penicillin: they inhibit cell wall synthesis by interacting with PBPs.
First-generation cephalosporins are primarily active against gram positive cocci. Newer cephalosporins have successively broader coverage against both gram positive and gram negative bacteria.
Cephalosporins can be substituted for penicillin in patients who are hypersensitive to penicillin, but they are not used in patients who have anaphylaxis to penicillins.
These include Vancomycin, Teicoplanin, Telavancin, Ramoplanin, and Decaplanin. They bind directly to the D-alanine D-alanine portion of the precursor peptidoglycan cell wall, blocking transpeptidase binding and inhibiting cell wall synthesis.
Vancomycin is the drug of choice for MRSA (Methicillin resistant S.aureus). It is effective against gram positive bacteria, including Staphylococci and Enterococci. Teicoplanin has a similar range of efficacy.
These include Imipenem, Meropenem, Doripenem, and Ertapenem. They are broad-spectrum bactericidal antibiotics effective against gram positive and gram negative bacteria, as well as anaerobes.
Imipenem is the drug of choice for Extended Spectrum Beta Lactamase (ESBL) producing gram negative bacilli.
Carbapenems bind to PBPs and inhibit bacterial cell wall synthesis.
This group includes Aztreonam, Tigemonam, Nocardicin A, and Tabtoxin. Their mechanism of action is like other beta lactam antibiotics. They are effective against aerobic gram negative bacteria only.
Cycloserine/Seromycin is used as a second-line drug for Tuberculosis. It is structurally similar to D Alanine, which is used to build D-Alanine D-Alanine in the bacterial cell wall. For that reason, cycloserine inhibits the enzymes alanine racemase and D-Alanine D-Alanine ligase, which inhibits cell wall synthesis.
Bacitracin is used topically to treat skin infections. It inhibits dephosphorylation of lipid carriers that transport peptidoglycan subunits across the cell membrane, thereby inhibiting cell wall synthesis.
Sign up for free to take 1 quiz question on this topic