They cause important human diseases such as streptococcal pharyngitis, rheumatic fever, endocarditis, and necrotising fasciitis, among others. The most important streptococci to know are beta-hemolytic streptococci, pneumococci, and Streptococcus viridans.
Streptococci are gram-positive cocci arranged in chains or pairs. Streptococcus pneumoniae (pneumococci) are classically seen as lancet (flame)-shaped diplococci in pairs.
S. pyogenes (beta-hemolytic strep) has a hyaluronic acid capsule. S. pneumoniae and GBS (group B streptococci such as S. agalactiae) have a polysaccharide capsule. Viridans streptococci do not have a capsule, but they produce a glycocalyx.
On the basis of the type of hemolysis produced on blood agar, streptococci may be classified as alpha hemolytic, which form a green zone of hemolysis due to incomplete breakdown of RBCs (e.g. S. viridans, S. pneumoniae); beta hemolytic, which produce a clear zone due to complete lysis of RBCs (e.g. S. pyogenes, S. agalactiae); and gamma hemolytic (non hemolytic), which do not lyse RBCs (e.g. many strains of S. bovis).
Group A streptococci are the most common cause of bacterial pharyngitis (strep throat), erysipelas (infection of dermal lymphatics presenting as a demarcated, raised, inflamed area usually on the cheeks), impetigo (honey-colored crusted lesions), necrotizing fasciitis (exotoxin B effect, “flesh eating bacteria”), streptococcal toxic shock syndrome, endometritis, sinusitis, and mastoiditis.

This image depicts an intraoral view of a patient, who had presented to a clinical setting exhibiting redness and edema of the oropharynx, and petechiae, or small red spots, on the soft palate. A diagnosis of strep throat had been made, caused by group A Streptococcus bacteria. These bacteria are spread through direct contact with mucus from the nose or throat, of persons who are infected, or through contact with infected wounds, or sores on the skin.
Some people with strep throat develop a red, sandpaper-like rash that blanches under pressure. It typically starts on the face and spreads over the body, and is accompanied by fever and sore throat. This presentation is called scarlet fever.

Scarlet fever rash on the volar surface of the forearm, due to group A Streptococcus bacteria.
S. pyogenes can also cause nonsuppurative diseases, namely acute rheumatic fever and acute post-streptococcal glomerulonephritis.
Acute rheumatic fever: Typically follows streptococcal pharyngitis by 1 to 5 weeks. It is due to immune cross-reactivity between M proteins on streptococci and human tissues, especially heart valves, joints, and the central nervous system. Clinical diagnosis is made using the revised Jones criteria.
Other useful antibody tests include anti-DNAse B, antistreptokinase, and antihyaluronidase.
| Major criteria | Minor criteria |
|---|---|
| Carditis, Polyarthritis (migratory), Chorea, Erythema marginatum, Subcutaneous nodules | Polyarthralgia, Fever. Elevated CRP, Elevated ESR, Prolonged PR interval |
Acute glomerulonephritis: Typically follows S. pyogenes skin infection (impetigo), or less commonly pharyngitis/scarlet fever, by 2-3 weeks. The responsible strains are called nephritogenic strains. The disease is due to deposition of immune complexes on the glomerular basement membrane. On biopsy, subepithelial humps are seen. It characteristically presents with periorbital edema, hypertension, and “smoky” urine from hematuria.
Pneumococci cause lobar pneumonia with reddish-brown or rusty sputum, otitis media, sinusitis, meningitis, and sepsis.
Group B streptococci cause neonatal sepsis and meningitis. Incidence can be reduced by maternal screening for GBS in the perinatal period.
Viridans streptococci (S. mutans, S. sanguis, S. mitis) are the most common cause of infective endocarditis. S. mutans causes dental plaque and caries. S. bovis is associated with endocarditis in older patients with colon cancer.
Streptococcus pyogenes: Gram-positive cocci in chains. The capsule is not stained by Gram stain, so it may appear as a halo around the bacteria. Throat swabs can be taken for Gram stain, rapid antigen testing, and culture. Gram stain of a throat swab is indeterminate because S. pyogenes looks morphologically similar to other throat commensals. Blood agar culture shows beta-hemolytic colonies that are inhibited by a bacitracin disc (bacitracin sensitive).
In streptococcal toxic shock syndrome, blood cultures are usually positive (unlike in staphylococcal TSS).
In a patient presenting with acute rheumatic fever, throat culture for streptococcus is usually negative (because the infection occurred a few weeks earlier).
Group B streptococci: Rectal and vaginal samples can be taken for Gram stain and culture. Rapid DNA testing can give results in an hour. They form beta-hemolytic colonies on blood agar, hydrolyze hippurate, are bacitracin resistant, and give a positive CAMP test.
Group D streptococci (EXCEPT Enterococci): They are alpha or non-hemolytic on blood agar. They characteristically hydrolyse esculin in the presence of bile, producing a black pigment on bile esculin agar. They do not grow in 6.5% NaCl.
Viridans streptococci: They are alpha hemolytic on blood agar, resistant to optochin, and resistant to bile lysis (not bile soluble).
Pneumococci: On Gram stain, they appear as gram-positive lancet-shaped diplococci (cocci in pairs) with a surrounding halo due to the capsule. They are alpha hemolytic on blood agar. They are characteristically sensitive to optochin and are bile soluble. The Quellung reaction can be used to detect pneumococci. Blood cultures are positive in about 20% of patients with pneumococcal pneumonia. A latex agglutination test on CSF can be done for rapid diagnosis of pneumococcal meningitis. Bacteremia and pneumonia can be indirectly detected by the presence of pneumococcal capsular antigen in urine.
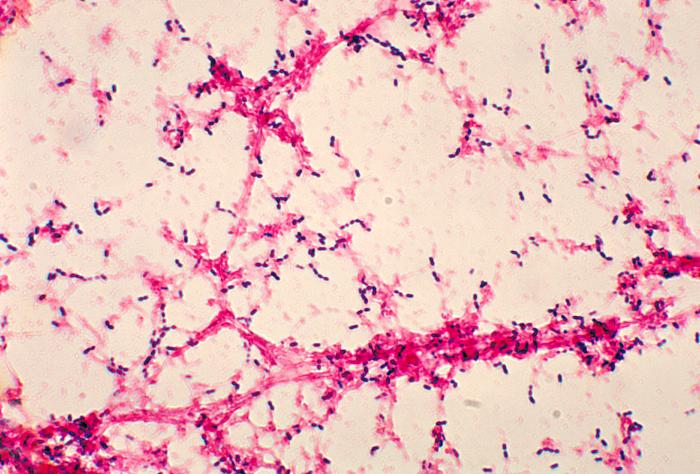
Numerous, Gram-positive, Streptococcus pneumoniae
Sign up for free to take 3 quiz questions on this topic