Fate of inflammation: Inflammation can have four different outcomes: resolution, healing, suppuration (pus and abscess formation), or chronic inflammation.
A) Chronic inflammation: You see chronic inflammation when acute inflammation persists or when pathogens such as Mycobacteria infect tissues. Macrophages are the most important cells in chronic inflammation. Most tissue macrophages are derived from blood monocytes. Macrophages are activated by cytokines and toxins. Once activated, macrophages release enzymes and cytokines that can cause tissue necrosis. Other important cells in chronic inflammation include lymphocytes, plasma cells, eosinophils, and mast cells. Lymphocytes and macrophages influence each other through cytokines and other mediators. Systemic amyloidosis may occur as a result of chronic inflammation.
i) Chronic granulomatous inflammation: This is a special type of chronic inflammation characterized by granuloma formation. A granuloma is a circumscribed, granule-like lesion made up chiefly of epithelioid cells, multinucleated giant cells, and lymphocytes. It may have necrotic areas in the center, with fibroblasts and fibrosis at the periphery.
Epithelioid cells are the most important component of a granuloma. They are modified macrophages, but they resemble epithelial cells: elongated shape, vesicular nucleus, and abundant pale cytoplasm. Multiple epithelioid cells can fuse to form multinucleated giant cells, which may have more than 20 nuclei. There are different types of giant cells:
CD4+ or CD8+ lymphocytes are present. Granulomatous inflammation is a type IV hypersensitivity reaction.
A characteristic granulomatous inflammation is seen in tuberculosis, with central cheese-like (caseous) necrosis and the appearance of granules called tuberculoma in infected tissues, along with Langhans’ type giant cells.

Mnemonic See A Scratchy TuberKLe. See for Syphilis/ A actinomycosis / Scratchy cat scratch disease/ Tuber Tuberculosis/ Tularaemia // K kleb granulomatis / Le leprosy
Non-infectious causes of granulomatous inflammation include sarcoidosis, berylliosis, vasculitis such as giant cell arteritis, Takayasu’s arteritis, Granulomatosis with polyangiitis (GPA), foreign bodies like talc and sutures, silicosis, and Crohn’s disease.

The antigen that triggers granulomatous inflammation typically can’t be completely destroyed by the immune system. As a result, the body walls it off from normal tissue by forming a granuloma. This is why tuberculosis can reactivate and cause reinfection later if the granuloma breaks down for any reason.
Macrophages are activated by gamma interferon and TNF alpha. Activated CD4+ cells and macrophages secrete cytokines with key functions as follows:
| Cytokine | Role in granuloma |
| IL1 and IL2 | Proliferation of T cells |
| Gamma interferon | Activates macrophages, activation of endothelium to promote CD4+ T cell adhesion, induces TNF secretion by macrophages |
| TNF alpha | Fibroblast proliferation, activates endothelium to secrete prostaglandins and increase adhesion, activates macrophages to kill intracellular pathogens, induction of apoptosis |
| IL 12 | Activation of NK cells and CD8+ T cells, induces gamma interferon production |
| Growth factors (TGF beta, PDGF) | Fibroblast proliferation |
TNF alpha and gamma interferon are essential for the formation and maintenance of a normal granuloma. Overexpression of TNF alpha causes tissue necrosis, cachexia, shock, and DIC.
Interferons alpha and beta are produced in response to viral infections: alpha by leukocytes and beta by fibroblasts. Gamma interferon is secreted in response to immune and inflammatory stimuli by activated T cells and NK cells.
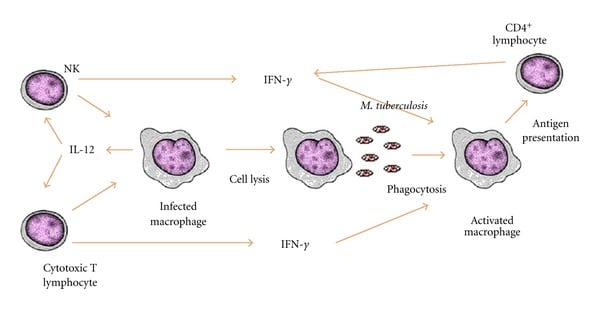
Initial protective response to M. tuberculosis-Th1 profile.
Sign up for free to take 4 quiz questions on this topic