The hormones of the anterior pituitary are controlled by hypothalamic hormones. The pituitary secretes hormones from the anterior and posterior lobes.
Anterior pituitary hormones: 6 major hormones are secreted by the anterior pituitary: FSH, LH, TSH, ACTH, GH, and prolactin. TSH, FSH, and LH are glycoproteins. Placental HCG is structurally similar to TSH, FSH, and LH. ACTH, MSH, beta lipotropin, and beta endorphin are derived from the same precursor molecule, pro-opiomelanocortin. For this reason, ACTH has properties similar to MSH and can lead to hyperpigmentation in Addison’s disease when ACTH is elevated.
Growth hormone: GH is synthesized by somatotrophs in the anterior pituitary. Somatotrophs are the most abundant cell population in the adult pituitary gland. GH is secreted in a pulsatile fashion. Secretion is increased during sleep, hypoglycemia, by ghrelin, at puberty, with arginine, exercise, stress, trauma, etc. Secretion is decreased in old age, obesity, with glucagon, etc.
Regulation of GH secretion: GHRH (GH-releasing hormone) from the hypothalamus increases GH secretion by activating a G protein-coupled receptor, resulting in increased cAMP, IP3, and Ca++. GH secretion is inhibited by the hypothalamic hormone somatostatin, which activates a Gi protein to decrease cAMP.
GH secretion shows three negative feedback mechanisms:
Estrogens, androgens, and ghrelin stimulate GH release.
GH actions: GH acts both directly through its own receptors and indirectly through induced production of IGF-I. GH receptors are present in many tissues, including fat, lymphocytes, liver, muscle, heart, kidney, brain, and pancreas.
Activation of receptor-associated Janus kinase (JAK)-2 is the critical step in initiating GH signaling. Phosphorylated residues on GHR and JAK2 form docking sites for different signaling molecules, including signal transducers and activators of transcription (STATs). STATs then translocate to the nucleus, where they bind to DNA and activate gene transcription. Cytokine-inducible suppressors of cytokine signaling (SOCS) suppress GH signaling by inhibiting JAK2 activity and competing with STAT.
GH stimulates synthesis of a peptide, IGF-I, in the liver and many other target tissues. Following binding of the IGF-I molecule, its receptor undergoes a conformational change that activates tyrosine kinase, leading to auto-phosphorylation of tyrosine. The activated receptor phosphorylates IRS-2, which in turn activates the RAS-activating protein SOS. This complex activates the MAPK (MAP kinase) pathway, leading to stimulation of cell growth.
GH stimulates lipolysis and promotes insulin resistance. It increases blood glucose levels. GH stimulates protein synthesis both directly and via IGF-I, insulin, or lipid intermediates. IGF 1 is responsible for the growth-promoting action of GH. It leads to increased organ and muscle size, increased linear growth, and increased anabolic activity.
Prolactin: Prolactin is synthesized by lactotrophs in the anterior pituitary. Prolactin is also produced in smaller amounts by other tissues, such as the brain and pregnant uterus. Production is increased in pregnancy and lactation.
Regulation of prolactin secretion: Prolactin secretion is inhibited by dopamine, while it is stimulated by TRH (thyrotropin-releasing hormone), estrogen, suckling, dopamine antagonists (antipsychotics), stress, and sleep. Prolactin inhibits its own secretion by stimulating the release of dopamine. Dopamine agonists like bromocriptine inhibit prolactin secretion.
Prolactin actions: The prolactin receptor is a type-I cytokine receptor that signals predominantly via the JAK2-STAT5 signaling pathway, similar to the growth hormone receptor.
During pregnancy, the mammary gland undergoes extensive ductal side-branching and alveolar budding, evolving into a milk-secreting gland. Prolactin contributes to both proliferation and differentiation of mammary tissue. Prolactin stimulates the production and secretion of milk. Prolactin levels are high during pregnancy, but lactation is inhibited by high levels of estrogen and progesterone.
Prolactin inhibits ovulation by inhibiting the release of GnRH (gonadotrophin) from the hypothalamus. Prolactin has other effects like proliferation of pancreatic beta cells, T cell activation, and tumorigenesis.
Posterior pituitary hormones: Antidiuretic hormone (ADH), also called vasopressin, and oxytocin are synthesized in the hypothalamus and secreted by nerve terminals in the posterior pituitary gland.
ADH, antidiuretic hormone or vasopressin or arginine vasopressin:** ADH is mainly produced by magnocellular neurons within the supraoptic nucleus of the hypothalamus. It has dual functions in osmotic and cardiovascular homeostasis.
Regulation of ADH secretion: Release of ADH is stimulated by hyperosmolarity of the plasma, which activates osmoreceptors in the hypothalamus. ADH is also secreted during hypovolemia or volume contraction.
The cardiovascular effect is coordinated by inputs from baroreceptors traveling via the vagus nerve to the CNS and relaying to the paraventricular and supraoptic nuclei of the hypothalamus. Angiotensin II, pain, nausea, hypoglycemia, nicotine, and opiates stimulate ADH secretion. ADH secretion is inhibited by hypo-osmolarity of the plasma, ethanol, alpha-adrenergic agonists, atrial natriuretic peptide, and hypervolemic states.
Actions: The actions of vasopressin (ADH) are mediated by stimulation of tissue-specific G-protein-coupled receptors (GPCR), classified into V1 vascular, V2 renal, V3 pituitary, and P2 purinergic receptors. Vasopressin’s signal is transmitted through both Gs and Gq, leading to increased levels of cAMP and IP3 and Ca++ respectively. Gq also activates the transcription factor nuclear factor-κB.
V1 receptors are found in high density on vascular smooth muscle and cause vasoconstriction by increasing intracellular calcium. Platelets also express V1; upon stimulation, this induces an increase in intracellular calcium, facilitating thrombosis. V1 receptors are also found in the kidney, where they occur in high density on medullary interstitial cells, vasa recta, and epithelial cells of the collecting duct. Vasopressin acts on medullary vasculature through V1 to reduce blood flow to the inner medulla without affecting blood flow to the outer medulla. Additionally, vasopressin selectively contracts efferent arterioles through the V1 receptor, thus increasing GFR.
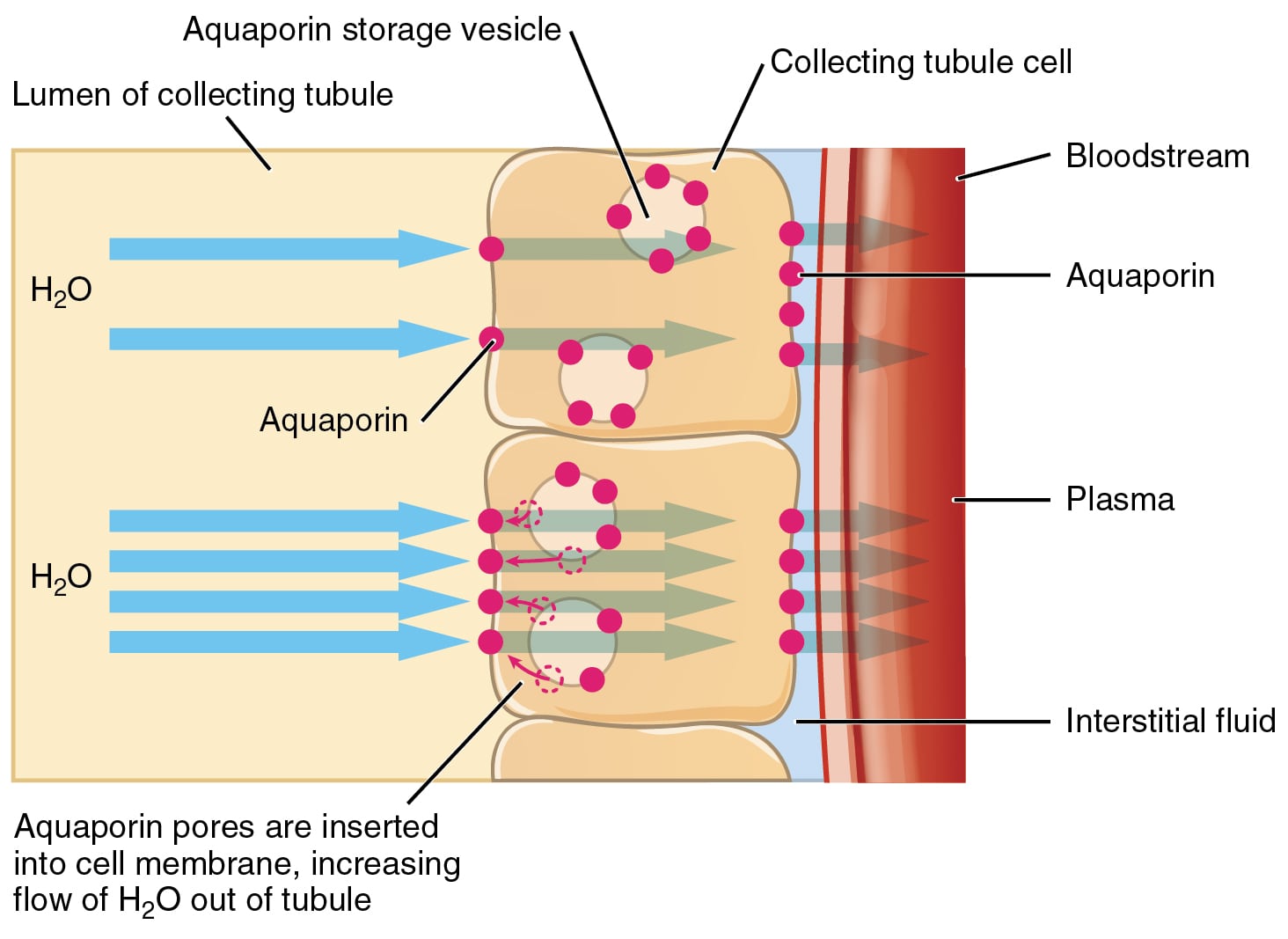
The antidiuretic effect of vasopressin occurs via activation of the V2 receptor located at the basolateral membrane of the late distal tubule and collecting ducts. V2 activates a Gs protein, leading to a rise in intracellular cAMP. Increased intracellular cAMP in the kidney triggers fusion of aquaporin-2-bearing vesicles with the luminal plasma membrane of the principal cells, increasing water reabsorption.
Oxytocin: Oxytocin is produced mainly by the paraventricular nucleus of the hypothalamus. Similar to ADH, it is released by nerve terminals into the posterior pituitary upon stimulation.
Regulation of oxytocin secretion: Suckling, and the sight, smell, or sound of the infant, as well as dilation of the cervix, are excitatory stimuli for oxytocin release. Opioids inhibit oxytocin release.
Actions of oxytocin: The oxytocin receptor is widely distributed. It is present not only on the myoepithelial cells surrounding the mammary ducts and uterine myometrium, but also in the olfactory processing regions of the brain, limbic system, and brainstem. Oxytocin receptors act through Gq, leading to a rise in intracellular Ca++.
Oxytocin causes milk ejection in lactating mothers by stimulating myoepithelial cells around the alveoli of the mammary glands. This is called “milk letdown”: milk already produced and stored under the action of prolactin is ejected by contraction caused by oxytocin.
Oxytocin also causes contraction of uterine smooth muscle and may play a role in initiation of labor. Oxytocin receptors are present in both the myometrium and parietal decidua of pregnant women. Oxytocin binding in decidua could mediate stimulation of prostaglandin synthesis, which would enhance oxytocin-induced contractions of the myometrium.
It has been postulated that oxytocin is involved in a wide array of social behaviors like maternal bonding, social decision-making and processing of social stimuli, and social memory.
Sign up for free to take 20 quiz questions on this topic