Enzymes and secretions
Various enzymes break down food into smaller molecules that your intestines can absorb. The table below summarizes the major enzymes involved in digestion.
| Enzymes present in saliva | ||
| Enzyme | Substrate | Digestion Products |
| Lingual lipase | Triglycerides | FFA*,mono and diglycerides |
| Salivary amylase | Polysaccharides | Di and trisaccharides |
| Gastric enzymes from chief cells of the stomach | ||
| Gastric Lipase | Triglycerides | FFA and monoglycerides |
| Pepsin | Proteins | Peptides |
| Small intestinal brush border enzymes | ||
| Enteropeptidase | Trypsinogen | Trypsin |
| Lactase | Lactose | Glucose and galactose |
| Maltase | Maltose | Glucose |
| Nucleosidases and phosphatases | Nucleotides | Nitrogen bases, phosphates and pentoses |
| Peptidases | Dipeptides and amino acids | Peptides and amino acids |
| Sucrase | Sucrose | Glucose and fructose |
| Pancreatic enzymes** | ||
| Carboxypeptidase | Amino acids at the carboxyl end | Amino acids |
| Chymotrypsin | Proteins | Peptides |
| Elastase | Proteins | Peptides |
| Nucleases | DNA and RNA | Nucleotides |
| Amylase | Polysaccharides | Alpha dextrins, maltose, maltotriose |
| Lipase | Triglycerides | FFA and monoglycerides |
| Trypsin | Proteins | Peptides |
*FFA stands for free fatty acids.
**Pancreatic enzymes are secreted in inactive zymogen form and must be activated first; exceptions are pancreatic amylase, lipase, and nucleases.
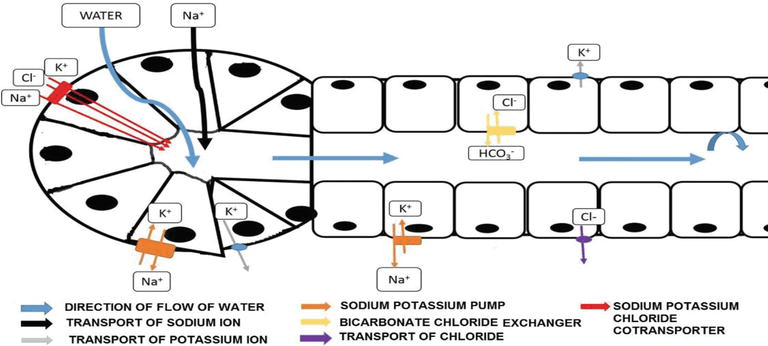
Secretion and composition of saliva: Salivary glands are organized into an acinus (where initial saliva is produced), followed by a short intercalated duct, and then a striated duct lined by ductal cells. Myoepithelial cells help move saliva through the ducts.
Parotid glands secrete more watery saliva and produce most saliva during tasting and chewing. Parasympathetic innervation to the parotid gland comes from the glossopharyngeal nerve (CN IX), originating in the inferior salivatory nucleus, and is relayed to the gland by the auriculotemporal nerve.
The sublingual and submandibular glands are supplied by the chorda tympani branch of the facial nerve. They secrete mixed serous and mucinous saliva and contribute more to resting (“background”) saliva that coats the oral surfaces between episodes of stronger stimulation.
Normally, saliva is hypotonic. Compared with plasma, it has:
- Higher K+ and HCO3-
- Lower Na+ and Cl-
Intercalated duct cells add lysozymes and lactoferrin to saliva. At higher flow rates, saliva more closely resembles plasma and also has a higher HCO3- concentration than at lower flow rates.
The salivary glands have both sympathetic and parasympathetic innervation. Both increase salivary secretion, although the composition differs. M1 and M3 are the main parasympathetic receptors, while alpha and beta are the main sympathetic receptors on the salivary glands. Parasympathetic stimulation increases IP3 and calcium, while sympathetic stimulation increases cAMP.
Factors affecting salivary secretion: Alpha adrenergic receptor stimulation produces high-protein secretion, while beta adrenergic or cholinergic stimulation produces lower protein but higher water and electrolyte secretion. Substance P stimulates both alpha adrenergic and cholinergic secretion of saliva. Parasympathetic stimulation produces copious watery saliva, while sympathetic stimulation produces thicker saliva. Antidiuretic hormone facilitates water reabsorption by the striated duct, aldosterone increases sodium reabsorption by the striated duct, and testosterone and thyroxine increase salivary secretion. In cystic fibrosis, saliva contains increased calcium levels, elevated Na+ and Cl-, and a decreased flow rate.
Gastric secretion: Parietal cells secrete HCl and intrinsic factor. Chief cells secrete pepsinogen. G cells secrete gastrin. Mucous cells in the oxyntic glands secrete mucus and pepsinogen. The low pH of the stomach helps convert inactive pepsinogen into active pepsin.
HCl secretion: The apical membrane of the parietal cell faces the gastric lumen, while the basolateral membrane faces the blood vessels. The apical membrane contains the H+K+ ATPase and Cl- channels. The basolateral membrane contains the Na+K+ ATPase and the Cl-HCO3- exchanger.
Carbonic anhydrase converts CO2 to H2CO3, which dissociates into H+ and HCO3-. H+ is actively secreted into the lumen by the H+K+ ATPase. HCO3- enters the bloodstream via the basolateral Cl-HCO3- exchanger, producing the post-meal “alkaline tide.” Cl- diffuses through apical Cl- channels into the gastric lumen and combines with H+ to form HCl.
H+ secretion is stimulated:
- Directly by ACh, histamine, and gastrin
- Indirectly by GRP (by increasing gastrin secretion)
These factors show potentiation: the combined effect of two factors is greater than the sum of their individual effects.
HCl secretion is also increased by distension of the stomach, products of protein digestion, alcohol, caffeine, and the acts of chewing, swallowing, and conditioned responses to smells.
Somatostatin inhibits HCl secretion by activating Gi, which inhibits adenylate cyclase and decreases intracellular cAMP. It also inhibits the release of histamine and gastrin.
The stomach protects itself from its own pepsin and HCl by producing mucus, HCO3-, prostaglandins, and growth factors. In gastric ulcers, net H+ secretion is low, while in duodenal ulcers H+ secretion is higher than normal.
Mchanism of increased H+ secretion by different factors
| Factor | Mechanism |
| Acetylcholine | Stimulation of M3 receptors; increase in intracellular IP3, DAG, calcium |
| Histamine | Acts through H2 receptors; increase in intracellular cAMP. |
| Gastrin | Acts through CCK B receptors on parietal cells; increases intracellular IP3 and calcium. |
Pancreatic secretion: The exocrine pancreas secretes enzymes in zymogen form. Parasympathetic stimulation increases pancreatic secretion, while sympathetic stimulation inhibits it. Pancreatic juice is high in Na+, Cl-, K +, and HCO3-. HCO3- neutralizes H+ from gastric chyme, which helps pancreatic enzymes function.
Secretion of HCO3- into the pancreatic lumen is associated with absorption of H+ into the pancreatic veins, which helps neutralize the post-meal alkaline tide. At higher flow rates, pancreatic juice has a higher HCO3- concentration and lower Cl-. The opposite occurs at lower flow rates. Na+ and K+ concentrations remain constant and are similar to plasma. Secretin stimulates HCO3–rich pancreatic secretion.
Liver, gallbladder and bile: Bile is continuously produced by hepatocytes. It is composed of 50% bile acids and bile salts, bile pigments, cholesterol, phospholipids, electrolytes, and water.
Cholic acid and chenodeoxycholic acid are the primary bile acids. Intestinal bacteria dehydroxylate them to form the secondary bile acids deoxycholic and lithocholic acids. The liver conjugates bile acids with the amino acids taurine and glycine to form bile salts, which makes them more water soluble. Bile salts emulsify dietary lipids and form micelles containing digested lipids.
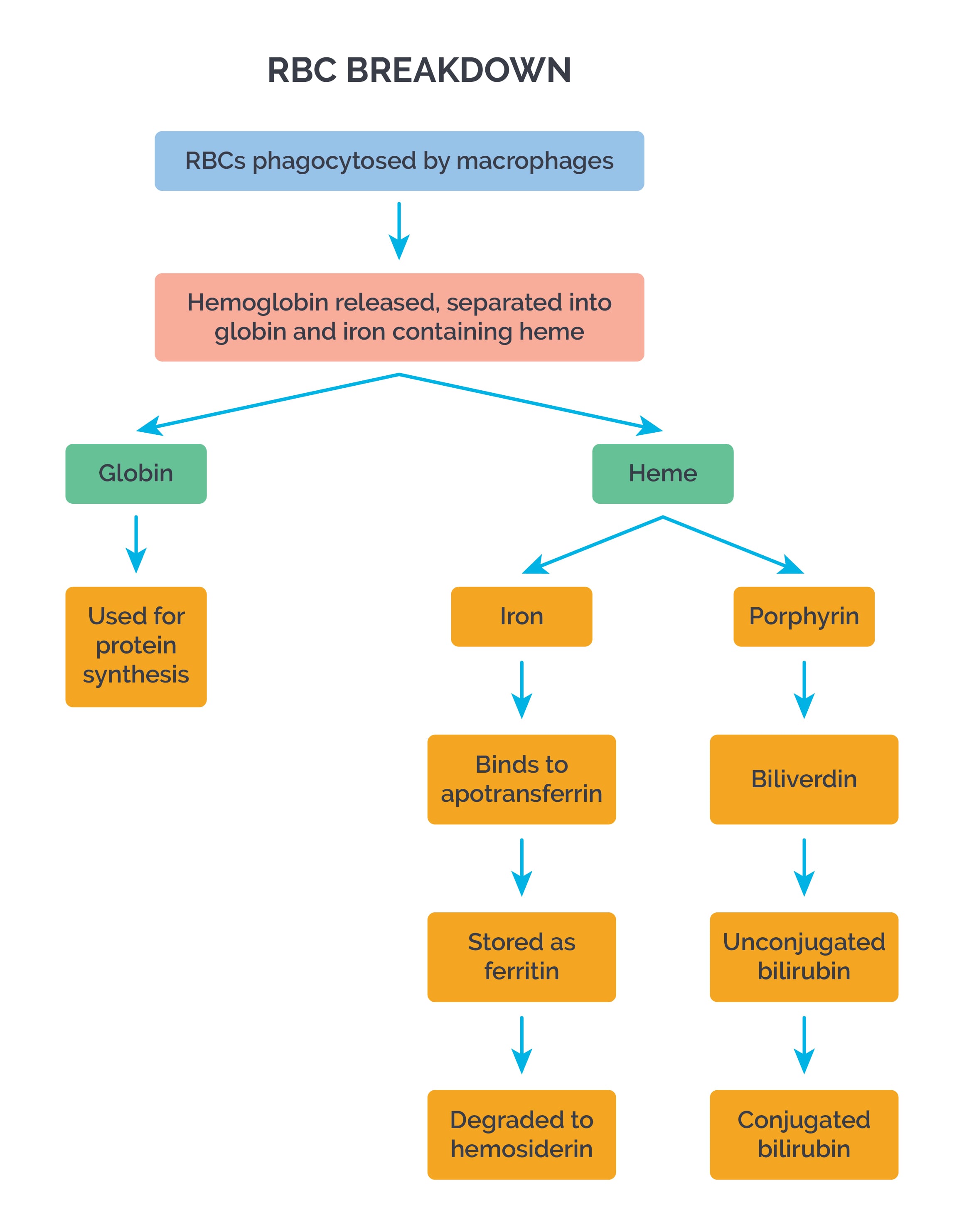
The major bile pigment is bilirubin. Reticuloendothelial cells form bilirubin from hemoglobin breakdown. Bilirubin travels to the liver bound to albumin. In the liver, UDP glucuronyl transferase conjugates bilirubin with glucuronic acid to form bilirubin glucuronide, which is secreted into bile.
In the intestine, bilirubin is freed and converted to urobilinogen by intestinal bacteria. Some urobilinogen is recirculated to the liver. Some is converted to urobilin and stercobilin, which give urine and feces their yellowish colors, respectively. Secretin stimulates secretion of electrolytes and water in bile.
Bile is stored in the gallbladder until CCK triggers bile ejection by causing gallbladder contraction and relaxation of the sphincter of Oddi. The longer bile is stored in the gallbladder, the more concentrated it becomes as water and ions are absorbed.
The liver performs many vital functions in the body. It plays an important role in carbohydrate, fat, and protein metabolism. It converts toxic ammonia to urea for excretion. It is a major site of detoxification reactions. It synthesizes almost all plasma proteins, including albumin and clotting factors.